Anterior pelvic tilt assessment
VOETBAL MEDISCH SYMPOSIUM 2020
DE BEHANDELING VAN VOETBALBLESSURES
PRAKTISCHE WETENSCHAP
OP DE KNVB CAMPUS IN ZEIST VINDT KOMEND JAAR OPNIEUW HET VOETBALMEDISCH SYMPOSIUM PLAATS.
HET SYMPOSIUM IS DÉ PLEK OM COLLEGA’S BINNEN HET VOETBALMEDISCHE DOMEIN TE ONTMOETEN OF KENNIS OP TE DOEN VAN GERENOMMEERDE EXPERTS. EN DIE NIEUWSTE INNOVATIES TE ZIEN OP HET GEBIED VAN VOETBALMEDISCHE EN FYSIEKE PRESTATIES.
NA VORIG JAAR DE DIAGNOSTIEK VAN VOETBALBLESSURES BELICHT TE HEBBEN, ROLT DE BAL DIT JAAR VERDER NAAR DE BEHANDELING VAN VOETBALBLESSURES. HET INHOUDELIJKE PROGRAMMA BIEDT OPNIEUW SPREKERS DIE ZICH ONDERSCHEIDEN IN ZOWEL DE DAGELIJKSE ZORG VOOR DE VOETBALLERS ALS OP WETENSCHAPPELIJK GEBIED.
VOETBAL MEDISCHE WORKSHOP 2020
(VELD)REVALIDATIE NA EEN VOETBALBLESSURE
OP 4 MAART ZAL ER WEDEROM EEN WORKSHOP PLAATS VINDEN BIJ HET KNVB VOETBAL MEDISCH CENTRUM.
OOK DIT JAAR BELOOFD HET EEN OCHTENDVULLEND PROGRAMMA TE ZIJN WAAR VOORNAMELIJK (SPORT)FYSIOTHERAPEUTEN HUN KENNIS MEE KUNNEN UITBREIDEN.
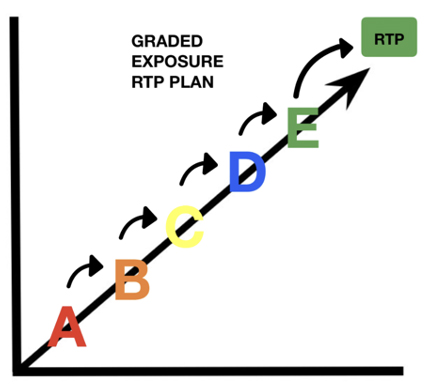
TIJDENS DE WORKSHOP ZAL MATT TABERNER ZIJN KENNIS EN EXPERTICE MET DE DEELNEMERS GAAN DELEN. MATT TABERNER IS EEN ERVAREN CLINICUS DIE AL JAREN EINDVERANTWOORDELIJK IS VOOR DE REVALIDATIE VAN TOPVOETBALLERS IN DE PREMIER LEAGUE. ZIJN FOCUS LIGT VOORNAMELIJK OP FYSIEKE ONTWIKKELING EN PRESTATIES. TEVENS IS HIJ DE ONTWIKKELAAR VAN HET ‘CONTROL-CHAOS CONTINUUM’.
DIT FRAMEWORK, WELKE VIJF FASES BESCHRIJFT HOE DE VELDREVALIDATIE NA EEN VOETBALBLESSURE OPGEBOUWD KAN WORDEN, STAAT CENTRAAL BINNEN DE WORKSHOP. DE THEORETISCHE ACHTERGROND,
DE TOEPASSING EN HET PRAKTISCHE ASPECT ZULLEN ALLEN AAN BOD KOMEN TIJDENS DE WORKSHOP.
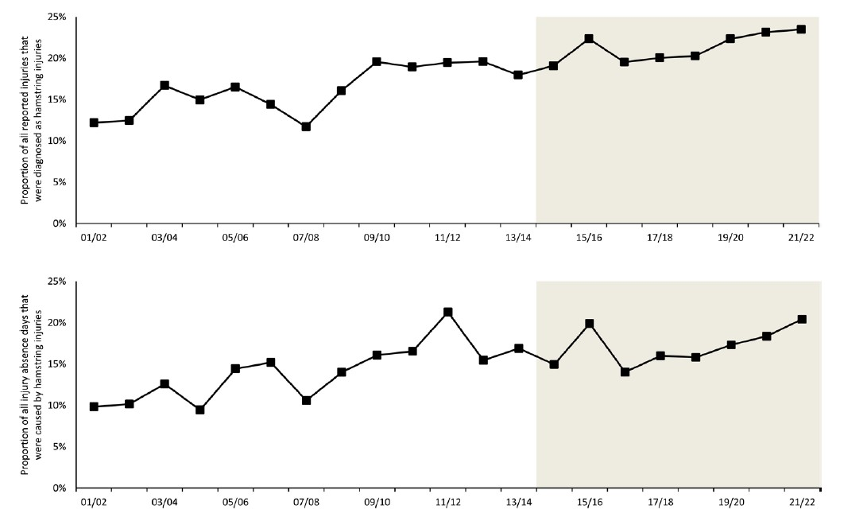
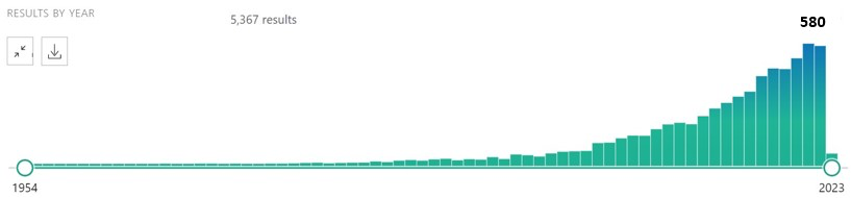
reviews

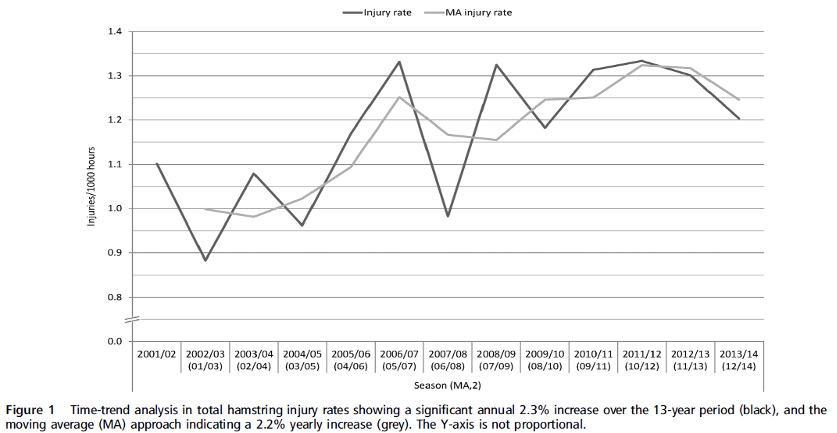
Nick van der Horst
Meet the soccerdoc
Nick van der Horst behaalde zijn diploma fysiotherapie in 2007 aan de Hogeschool Utrecht. Hij werkte 10 jaar lang als sportfysiotherapeut/echografist/docent bij het Academie Instituut te Utrecht. Daarna heeft hij de overstap gemaakt naar waar zijn hart ligt, het professionele voetbal. Hij heeft twee jaar als sportfysiotherapeut en hoofd van de medische staf bij Go Ahead Eagles in Deventer gewerkt. Momenteel is is Nick werkzaam bij de KNVB. Zijn onderzoeks-activiteiten zijn gefocust op de voetbal-medische zorg. In 2017 behaalde hij zijn doctoraal na het verdedigen van zijn proefschrift ‘Prevention of hamstring injuries in male soccer’.

Blogger: Raúl Gómez
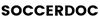
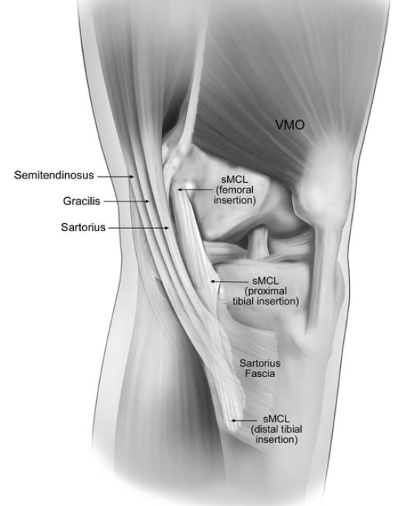
Correct pelvic alignment – Posture assessment
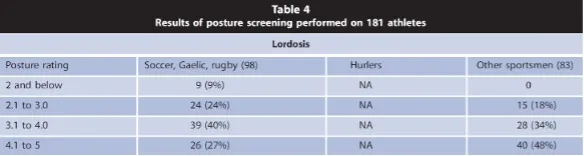
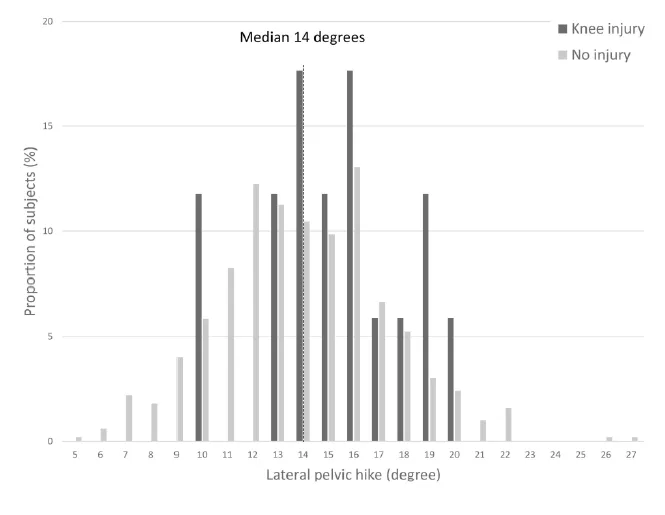
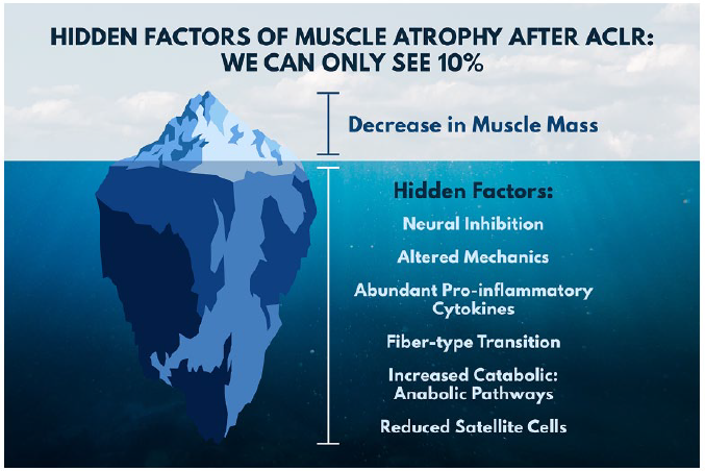
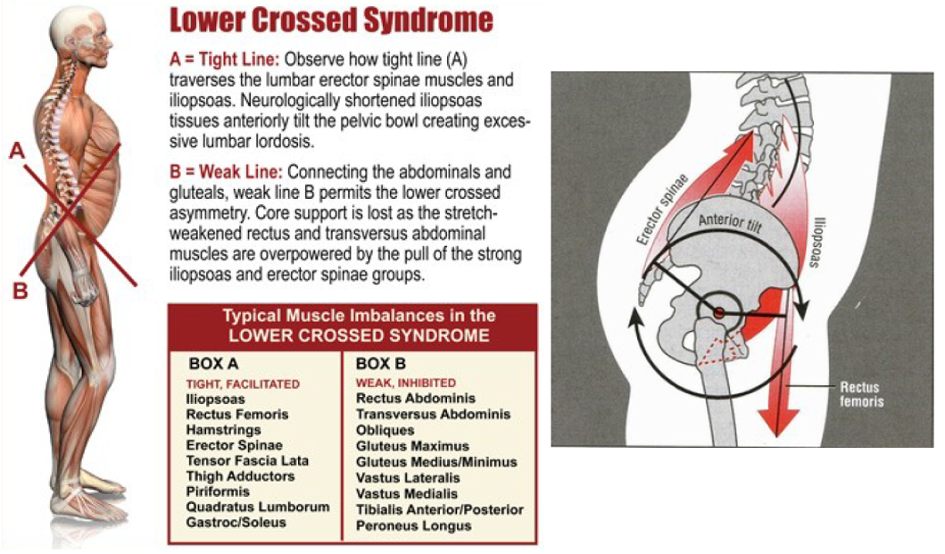
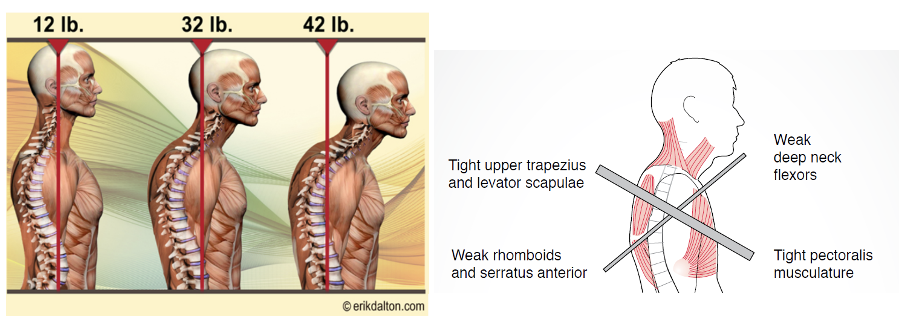
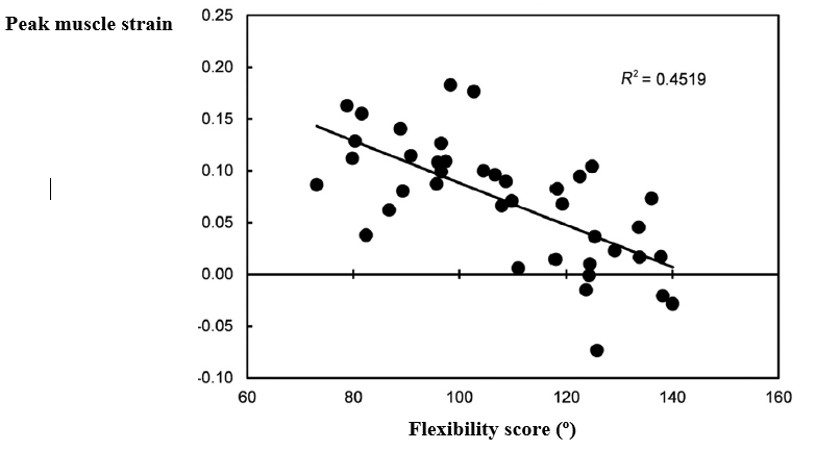
Although there is controversy regarding the analysis of static posture and its relationship with injuries during sports movements, certain postural patterns can provide valuable information about certain players’ predispositions to injury.
Recent studies have highlighted the role of excessive anterior pelvic tilt (APT) in increasing the risk of hamstring (Mendiguchia, et al., 2021) and hip injuries (Suits, 2021) and low back pain (Das, et al., 2017). However, the field is still evolving, and there are no cut-off values for the degree of pelvic tilt and its relationship to the most common injuries in football.
Suits (2021) defined pelvic tilt as the angle formed by a horizontal line and a line that separates the anterior superior iliac spine and the posterior superior iliac spine in the sagittal plane (see Image 1). He also presented in his article the findings of several articles that measured the pelvic tilt angle in healthy subjects, showing results ranging from 8º to 13º APT. This indicates that APT is a natural anatomical position and not inherently harmful. However, problems can arise when excessive APT occurs, particularly during high-intensity running.

Image 1. Pelvic tilt
Falk et al. (2020) set a cut-off value of 8° for APT, considering a higher degree excessive. However, the previous review by Suits (2021) suggests that this
cut-off value may be too low. Additionally, in healthy populations, women may exhibit a higher degree of APT than men (11.7° vs. 9.6°) (McKeon & Hertel, 2009).
In a 2013 study, Barbosa et al. compared the impact of a treatment involving manipulation of the sacroiliac joint and strength training of knee flexors and extensors on the degree of APT and subjective pain in 7 patients with low back pain. The results demonstrated a reduction of more than 5 degrees in APT (from 20.38 degrees to 14.63 degrees), which also led to a significant decrease in pain as indicated by subjective pain scale measurements (from 5.83 to 1.29).
Can we classify an APT greater than 13 degrees as a faulty postural pattern that increases the risk of injury in soccer players?
We can only make assumptions at this point, as no articles have studied the degree of APT and its association with injuries in football.
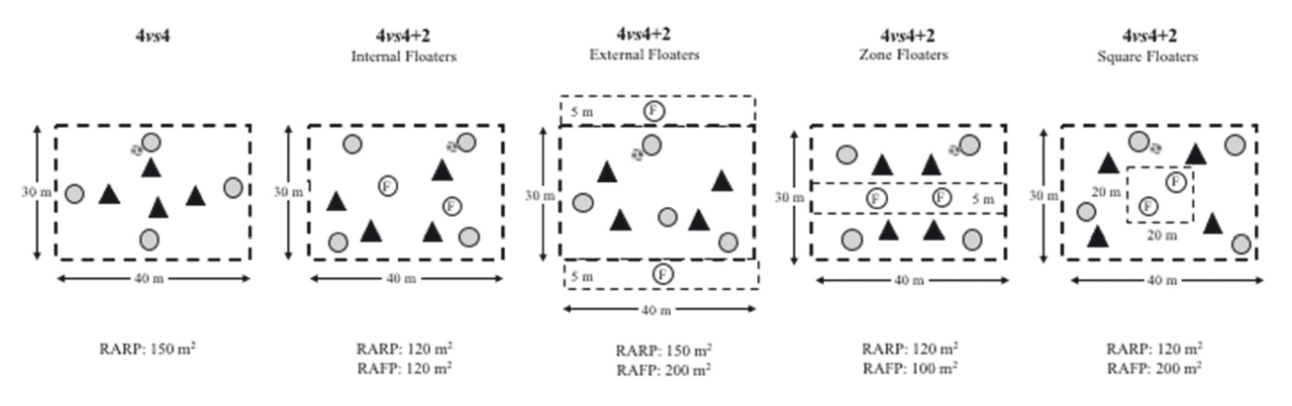
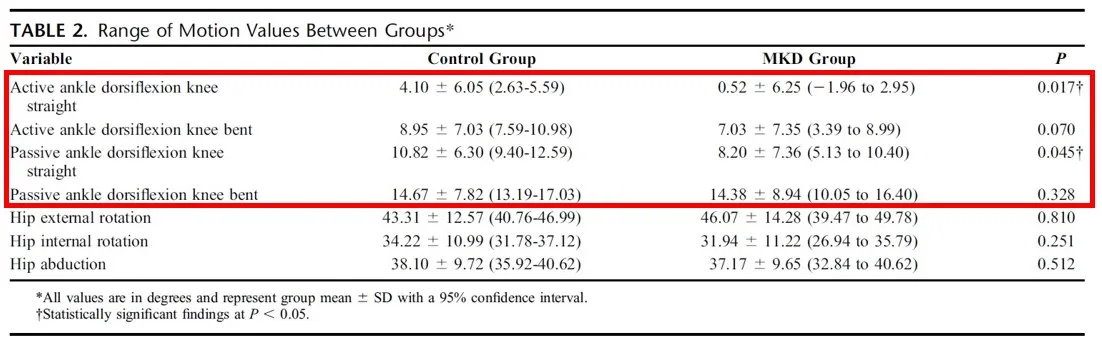
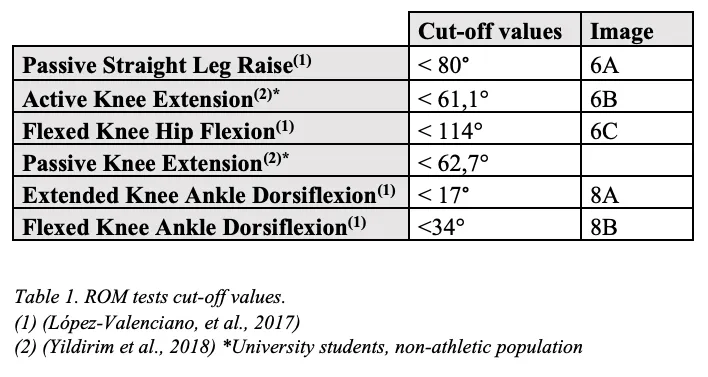
Range of motion
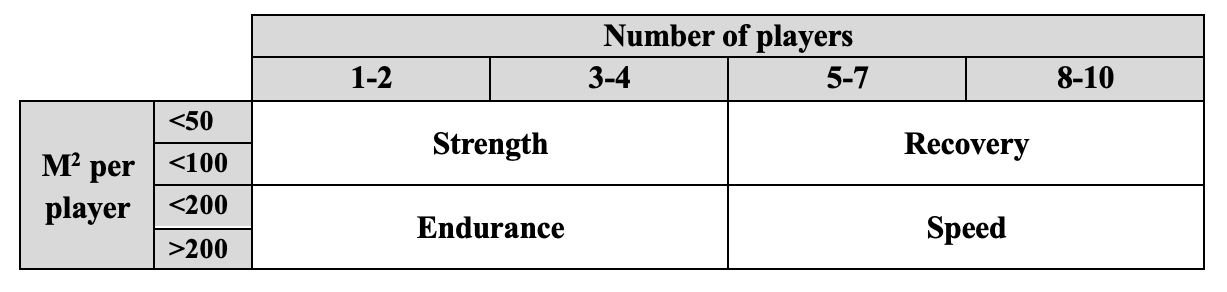
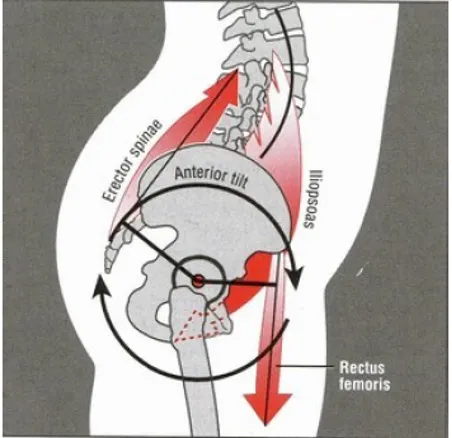
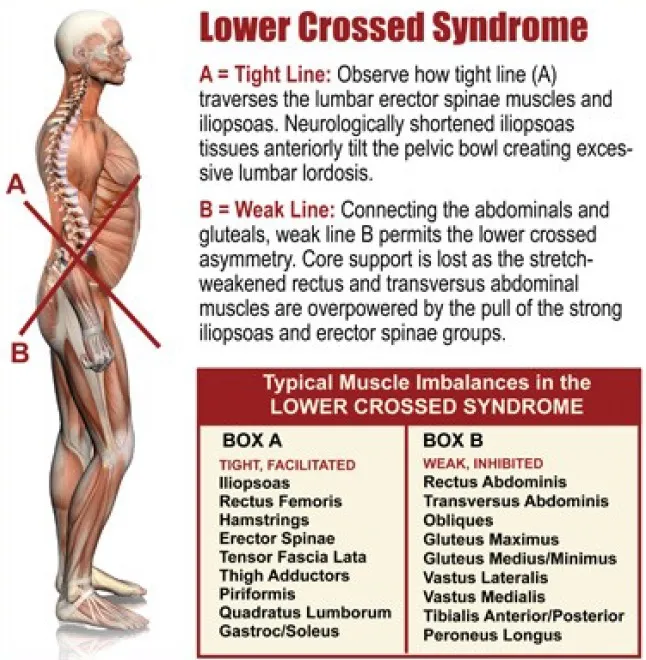
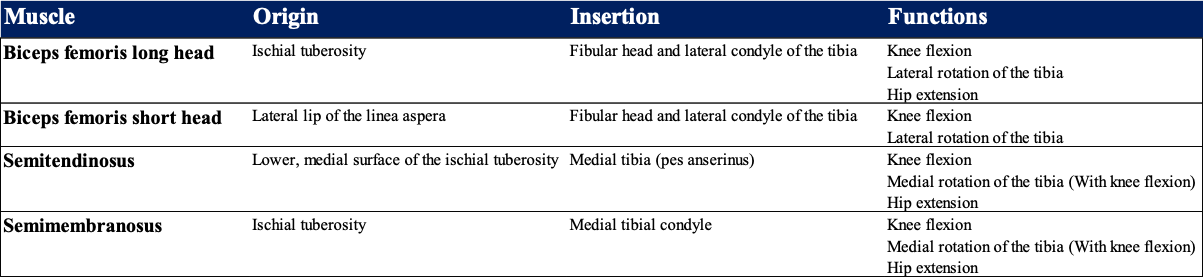
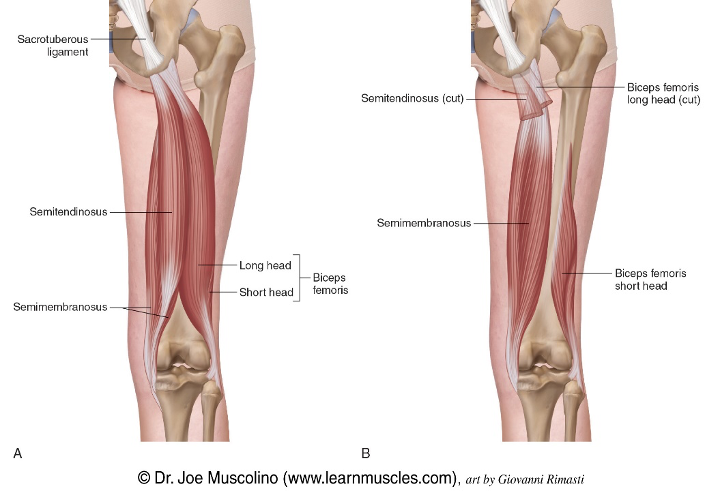
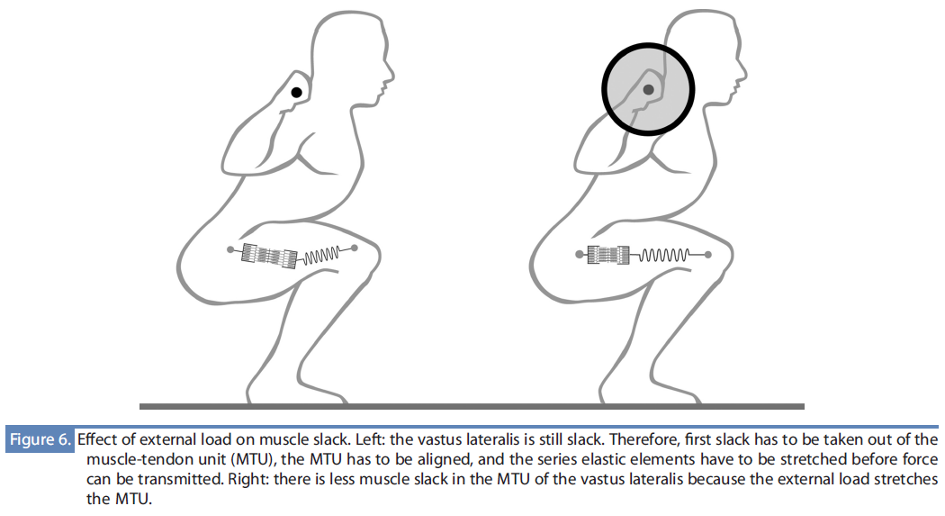
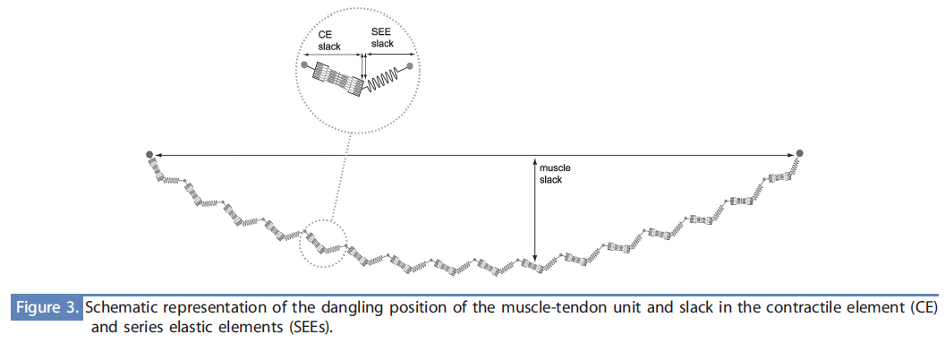
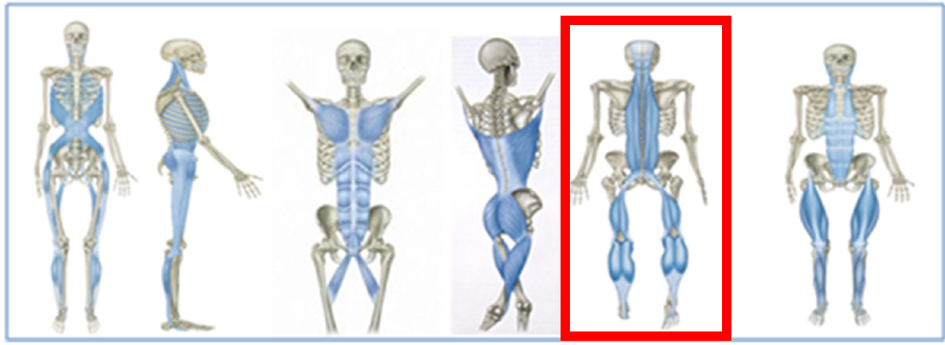
If the hip flexors are excessively tight and not adequately stabilized, they can cause the pelvis to rotate forward (Neumann, 2010). Table 1 lists the muscles that can potentially function as hip flexors and consequently increase APT.
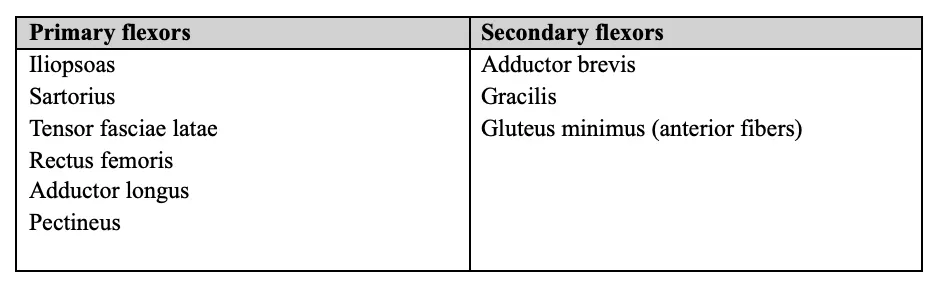
Table 1. Musculature involved in hip flexion (Neumann, 2010)
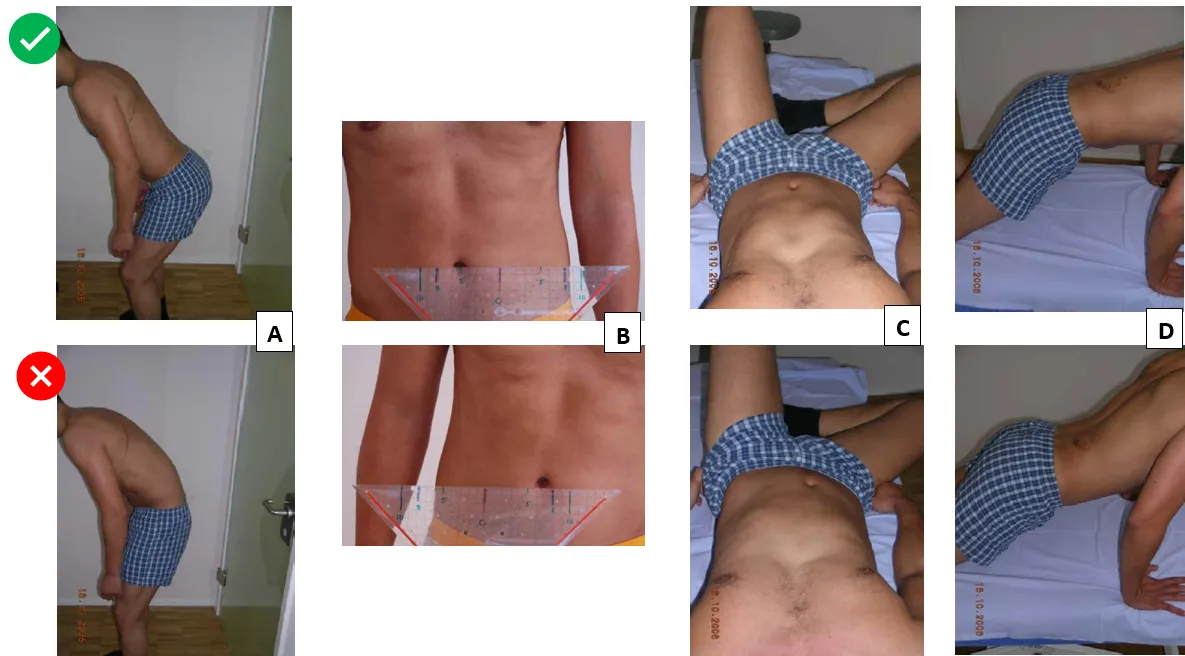
Modified Thomas Test
The procedure starts with the individual sitting at the edge of the table and lying back. Then, they should flex both hips as much as possible and hold their legs behind the knees in the popliteal area. Finally, they need to relax and extend one leg while still holding the other firmly in the fully flexed position (see Image 2).
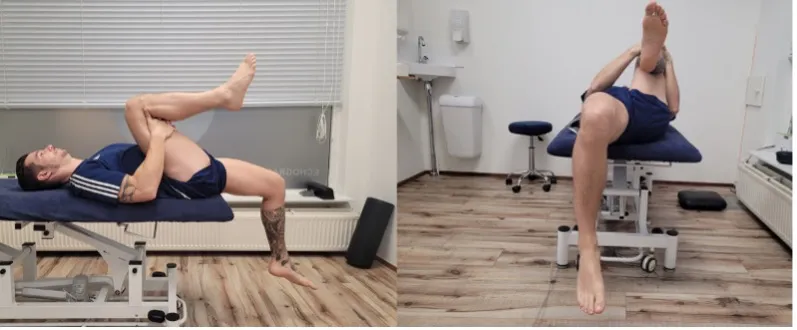
Image 2. Modified Thomas Test
The inability to maintain a neutral back position, arching the lower back, often indicates excessive shortening of the Psoas major.
This shortening can also result in an inability to fully extend the hip (Image 3).

Image 3. Hip extension restriction
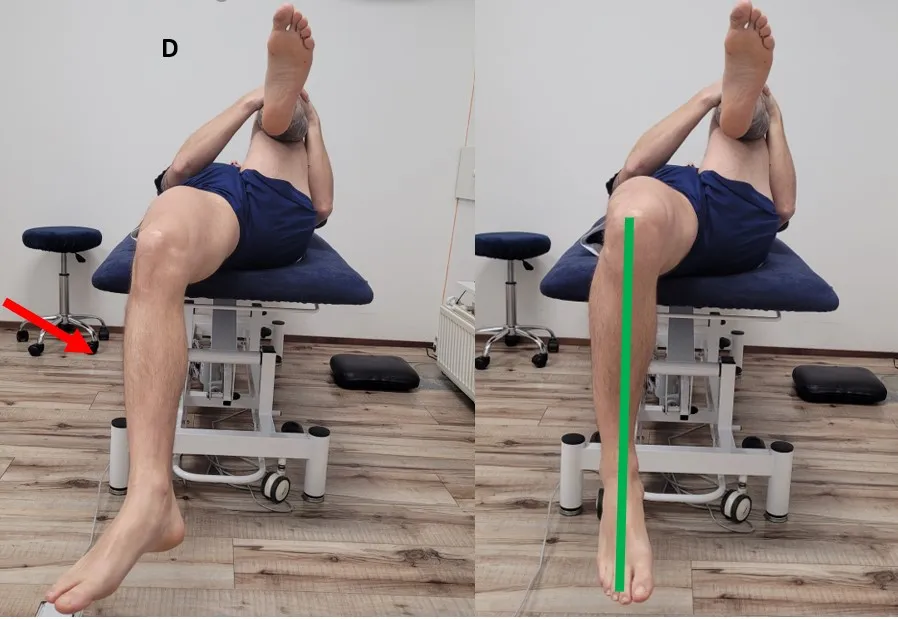
If the inability to fully extend the hip is accompanied by external rotation of the knee (Image 4, right), our biggest suspect will be the TFL. We can check this by passively adducting the extended leg (Image 4, left). An increase in external rotation of the knee will indicate excessive tension of the TFL and the iliotibial band (Neumann, 2010).

Image 4. Modified Thomas Test – Knee external rotation. (Sahrmann, 2002)
Another very common pattern is a lack of knee flexion (Image 5). Due to its biarticular nature, the rectus femoris can limit hip extension and knee flexion. Excessive tension of this muscle will cause the knee to extend, which, with correct mobility, should be perpendicular to the ground (Image 2).

Image 5. Knee extension restriction
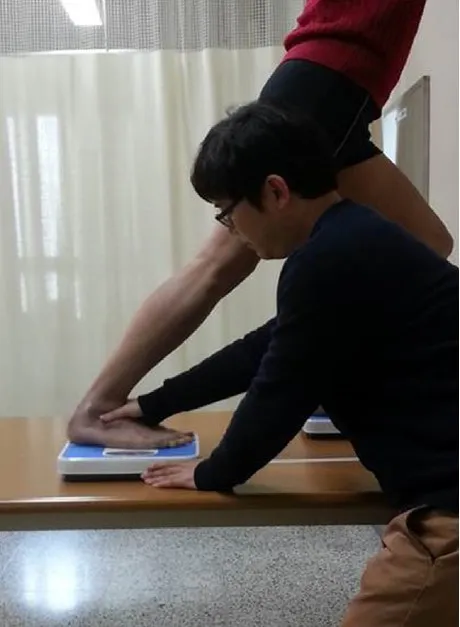
Jurdan Test
This test was first used in injury risk research in 2022 by Lahti et al. The test aims to assess the influence of the muscles of the lumbopelvic region on hamstring flexibility. The Jurdan test can be considered a combination of the active knee extension test and the modified Thomas test (Lahti, et al., 2022). The result of this test is defined as the difference between the shin angle of the actively lengthened leg and the thigh angle of the opposite leg (Image 6).
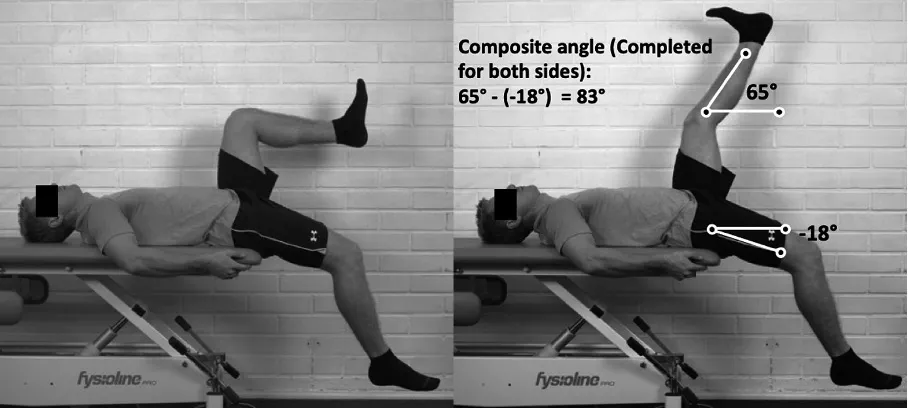
Image 6. Jurdan Test (Lahti, et al., 2022)
Although both the modified Thomas Test and the Jurdan test can provide a lot of information about hip range of motion, more research is still needed to determine cutoff values and their relation with lower limb injuries.
Strength
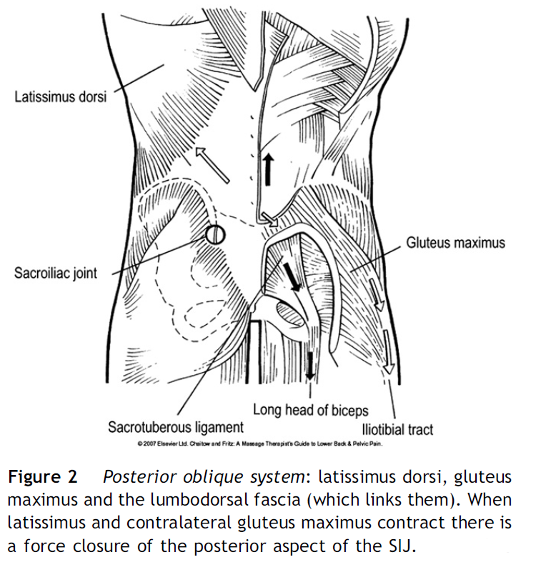
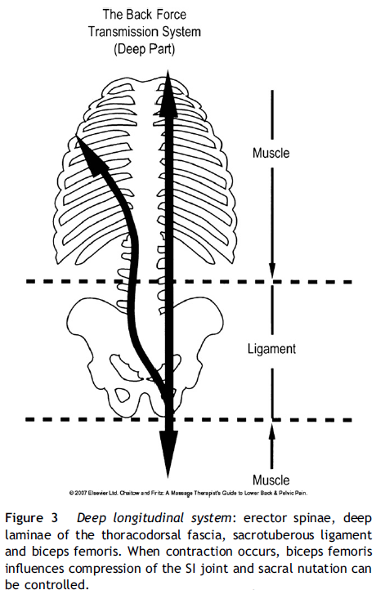
The abdominal muscles must generate a strong stabilizing force to counteract the strong APT caused by the hip flexors. This stabilizes the lumboabdominal region by increasing intra-abdominal pressure and thoracolumbar fascia tension (Neumann, 2010).
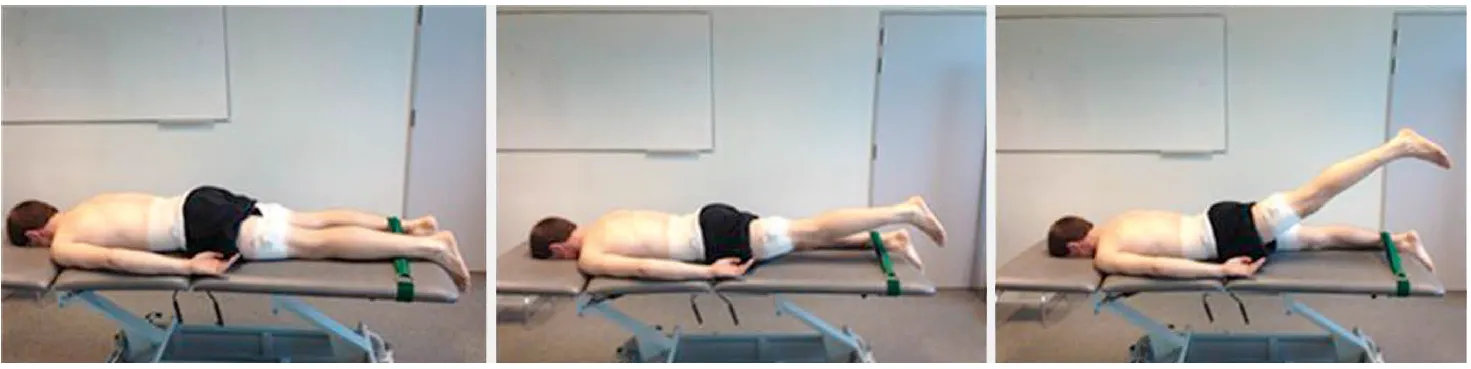
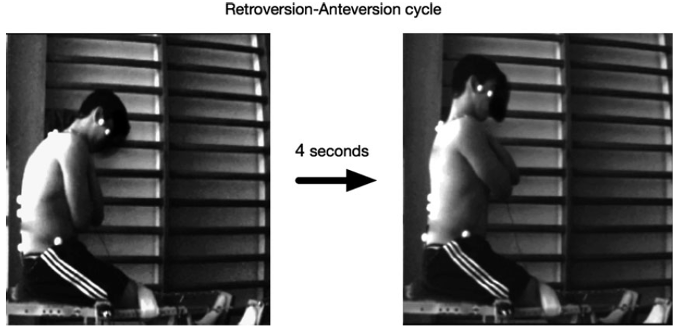
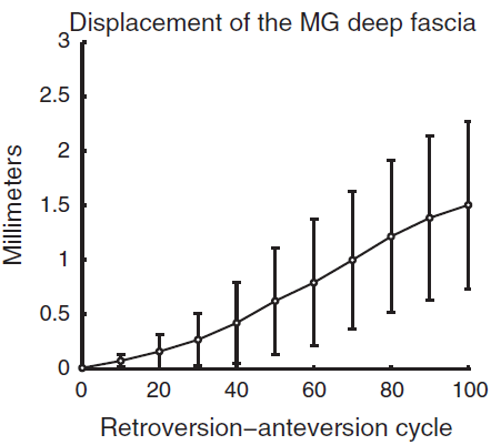
To assess the strength of the abdominal musculature against APT, Haladay et al. (2014) studied the results of the Double Limb Lowering Test* (DLLT) (Image 7) and Lower Abdominal Muscle Progression* (LAMP) (Image 8) after an abdominal stabilization exercise program. They found that the LAMP test is more sensitive to change after abdominal stabilization programs. However, no subject was able to reach the “normal” range of motion in the DLLT test as it was found to be too demanding. It is important to note that this study had some limitations, including a small number of participants (only 11), the inclusion of subjects of different genders, and varying levels of physical activity. In sports with physically demanding requirements such as football, athletes should be able to perform either of these tests with maximum results.
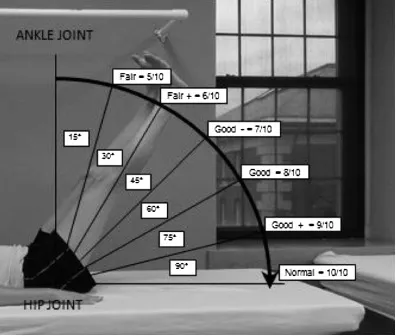
Image 7. DLLT. The subject lays supine and raises their legs to a position of 90º of hip flexion with the knees extended. They are then instructed to maintain their pelvis in a posterior pelvic tilt by contracting the abdominals while slowly lowering the legs to the supporting surface. Strength is graded, from 5/10 to 10/10, by identifying the point at which the subject was last able to keep the pelvis stable, as assessed by an anterior tilt of the pelvis and arching of the back (Haladay, et al., 2014).
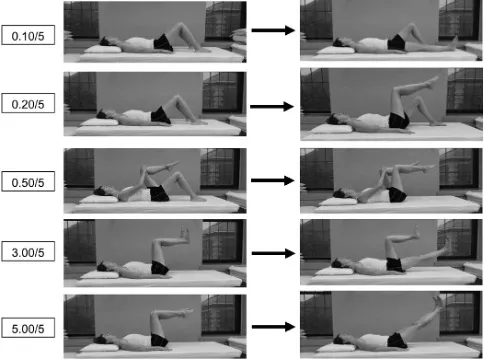
Image 8. The subject lays supine and performs a series of 9 progressively more challenging lower extremity combinations of movements, assessing their ability to stabilize the pelvis. During this test, the subject is instructed to contract their abdominal muscles by pulling their navel toward their spine. They are assigned a grade (0.10 through 5.00/5.00) for the most challenging lower extremity movement they are able to complete without motion on their pelvis or lower back (Haladay, et al., 2014).
* More information about these tests can be found in the following references: (Haladay, et al., 2014); (Sahrmann, 2002)
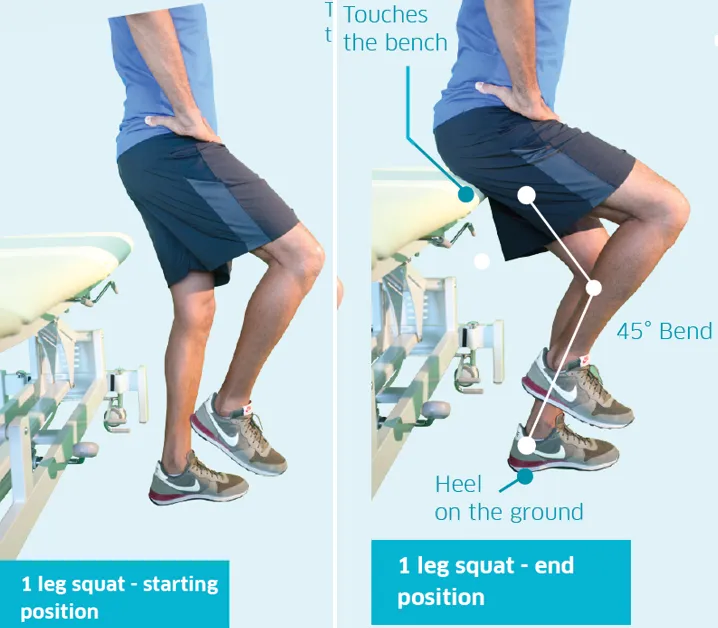
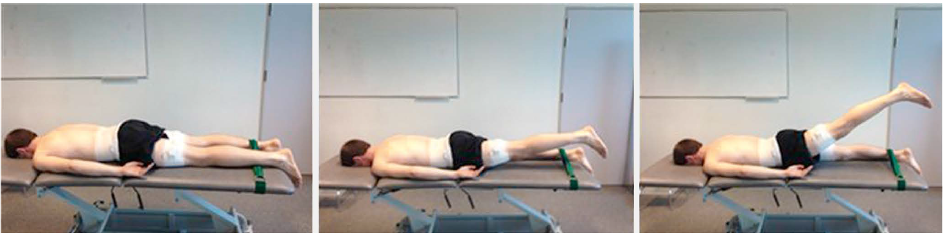
In a previous blog, we discussed the importance of the gluteus maximus (GM) muscle in correcting APT. According to Buckthorpe et al. (2019), there are various ways to assess GM strength. They affirm the prone hip extension task with the knee flexed at 90º as the most commonly used assessment and suggest using a dynamometer to measure it. Other assessment methods include isometric or isokinetic assessment. Electromyography is the most commonly used method to measure muscle activation.
Although all of these methods provide objective and reliable data, many teams may not have the necessary equipment or time to perform them.
The Single-Leg Glute Bridge Test (Image 9) offers an alternative that requires no equipment and can be done with the entire team at the same time in just a few minutes.

Image 9. Single-leg glute bridge
During this test, footballers are asked to perform as many repetitions as possible in the single-leg glute bridge exercise. After the test, the following data is recorded:
Maximum number of repetitions per leg – This will indicate whether there is an imbalance in the strength of the lower limb in unilateral hip extension.
Muscle that has suffered the greatest fatigue during the test – This test will determine if the muscle activation pattern of hip extension is functionally efficient. At the end of the test, it is normal to feel that fatigue in the GM has been the limiting factor of the exercise. I can assure you that you will strongly feel a “burning” sensation in that muscle if the test is carried out to failure. If other muscles, such as the quadriceps or hamstrings, are limiting the test result, this will indicate that the GM is not functioning correctly, and other muscles may be compensating for its weakness, known as synergistic dominance.
Muscle cramps or pain that may have limited the test result – Cramps in the hamstrings or back pain may indicate again weakness in the gluteus maximus and provide insight into other overloaded muscle groups due to lack of glute activation.
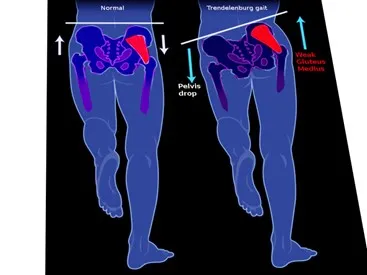
Motor control
Hip flexion-extension pattern
This is especially important in young players. Correctly teaching lumbopelvic dissociation is crucial, assuring that the footballer has perfect control over the motion of his/her hip without any compensation at the lumbar level. In a previous blog post, “Hamstring injuries – Post injury evaluation”, you can find several examples for the evaluation of lumbopelvic motor control.
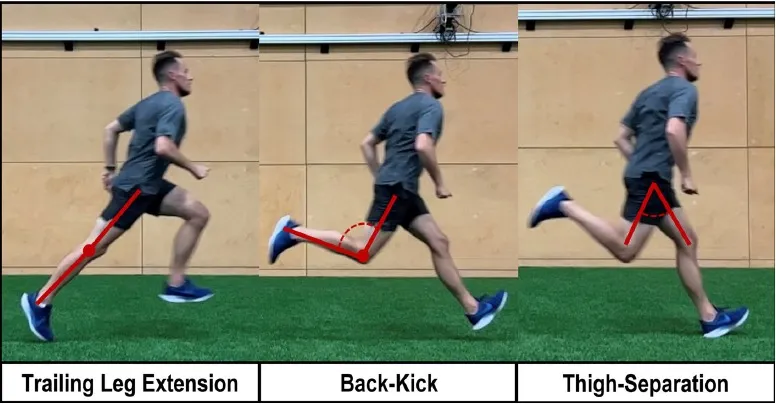
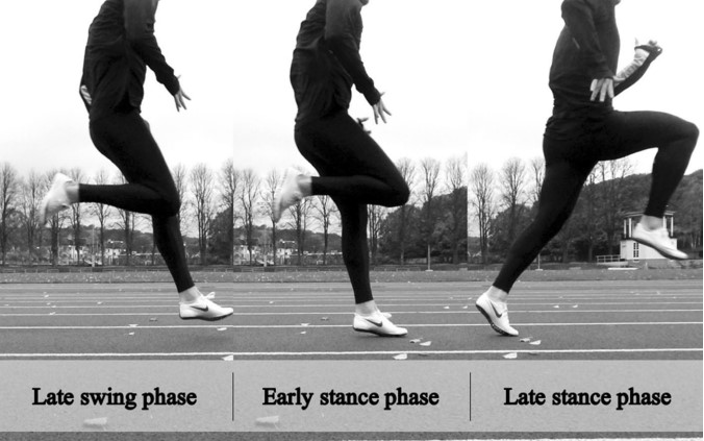
Sprint technique
Excessive APT during sprinting increases the risk of hamstring injuries. Correcting this movement pattern is crucial. This year, the reliability of the Sprint Mechanics Assessment Score (S-MAS) was evaluated, showing it to be a reliable tool for assessing sprint mechanics in football players (Bramah et al., 2024). I recommend reading the full assessment. In this post, we will only describe the most important points for footballers who present excessive APT.
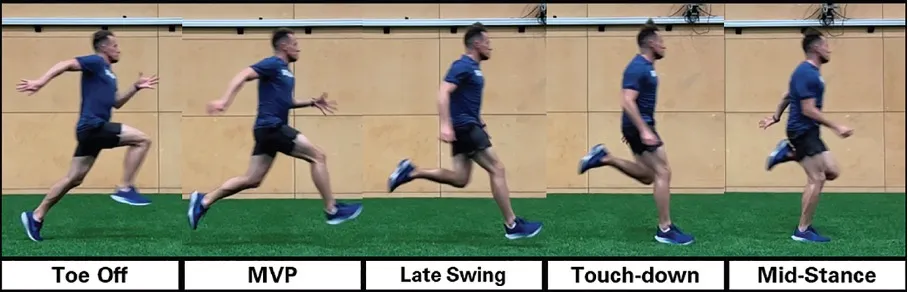
Image 10. Phases of sprint cycle. MVP – Maximal vertical projection (Bramah, et al., 2024)

Table 2. Phases of sprint cycle (Bramah, et al., 2024)
Although injury prevention is multifactorial in nature, correct and efficient movement plays a key role. Human movement is highly complex, but mastering specific motor patterns can substantially lower the risk of injury. We will soon delve into training these patterns and achieving a proper balance of muscular forces in the lumbopelvic area.
References
Barbosa, A., Martins, F., Barbosa, M. & Dos Santos, R., 2013. Manipulation and selective exercises decrease pelvic anteversion and low-back pain: A pilot study. Journal of Back and Musculoskeletal Rehabilitation, Volumen 26, pp. 33-36.
Bramah, C. y otros, 2024. The Sprint Mechanics Assessment Score – A Qualitative Screening Tool for the In-field Assessment of Sprint Running Mechanics. The American Journal of Sports Medicine, 20(10), pp. 1-9.
Buckthorpe, M., Stride, M. & Della Villa, F., 2019. Assessing and treating gluteus maximus weakness – A clinical commentary. The International Journal of Sports Physical Therapy, pp. 655-670.
Das, S. y otros, 2017. Prevalence of lower crossed syndrome in young adults: a cross sectional study. International Journal of Advanced Research, 5(6), pp. 2217-2228.
Falk, A., Overgaard, S., Hróbjartsson, A. Holsgaard, A., 2020. Non-surgical interventions for excessive anterior pelvic tilt in synptomatic and non-symptomatic adults: A systematic review. Efort Open Reviews, Volumen 5.
Haladay, D., Miller, S., Challis, J. & Denegar, C., 2014. Responsiveness of the double limb lowering test and lower abdominal muscle progression to core stabilization exercise programs in healthy adults: A pilot study. The Journal of Strength and Conditioning Research, 28(7), pp. 1920-1927.
Lahti, J., Mendiguchia, J., Edouard, P. & Morin, J.-B., 2022. A novel multifactorial hamstring screening protocol: association with hamstring muscle injuries in professional football (soccer) – a prospective cohort study. Biology of sport, 39(4), pp. 1021-2031.
McKeon, J. Hertel, J., 2009. Sex differences and representative values for six lower extremity alignment measures. Journal of Athletic Training, 44(3), pp. 249-255.
Mendiguchia, J. y otros, 2021. Can we modify maximal speed running posture? Implications for performance and hamstring injury management. International Journal of Sports Physiology and Performance.
Neumann, D., 2010. Kinesiology of the hip: A focus on muscular actions. Journal of orthopaedic & sports physical therapy, 40(2), pp. 82-94.
Neumann, D., 2010. Kinesiology of the musculoskeletal system. 2nd ed. Missouri: Mosby.
Sahrmann, S., 2002. Diagnosis and Treatment of Movement Impairment Syndromes. 1st ed. Missouri: Mosby.