Hamstring injuries in football
VOETBAL MEDISCH SYMPOSIUM 2020
DE BEHANDELING VAN VOETBALBLESSURES
PRAKTISCHE WETENSCHAP
OP DE KNVB CAMPUS IN ZEIST VINDT KOMEND JAAR OPNIEUW HET VOETBALMEDISCH SYMPOSIUM PLAATS.
HET SYMPOSIUM IS DÉ PLEK OM COLLEGA’S BINNEN HET VOETBALMEDISCHE DOMEIN TE ONTMOETEN OF KENNIS OP TE DOEN VAN GERENOMMEERDE EXPERTS. EN DIE NIEUWSTE INNOVATIES TE ZIEN OP HET GEBIED VAN VOETBALMEDISCHE EN FYSIEKE PRESTATIES.
NA VORIG JAAR DE DIAGNOSTIEK VAN VOETBALBLESSURES BELICHT TE HEBBEN, ROLT DE BAL DIT JAAR VERDER NAAR DE BEHANDELING VAN VOETBALBLESSURES. HET INHOUDELIJKE PROGRAMMA BIEDT OPNIEUW SPREKERS DIE ZICH ONDERSCHEIDEN IN ZOWEL DE DAGELIJKSE ZORG VOOR DE VOETBALLERS ALS OP WETENSCHAPPELIJK GEBIED.
VOETBAL MEDISCHE WORKSHOP 2020
(VELD)REVALIDATIE NA EEN VOETBALBLESSURE
OP 4 MAART ZAL ER WEDEROM EEN WORKSHOP PLAATS VINDEN BIJ HET KNVB VOETBAL MEDISCH CENTRUM.
OOK DIT JAAR BELOOFD HET EEN OCHTENDVULLEND PROGRAMMA TE ZIJN WAAR VOORNAMELIJK (SPORT)FYSIOTHERAPEUTEN HUN KENNIS MEE KUNNEN UITBREIDEN.
TIJDENS DE WORKSHOP ZAL MATT TABERNER ZIJN KENNIS EN EXPERTICE MET DE DEELNEMERS GAAN DELEN. MATT TABERNER IS EEN ERVAREN CLINICUS DIE AL JAREN EINDVERANTWOORDELIJK IS VOOR DE REVALIDATIE VAN TOPVOETBALLERS IN DE PREMIER LEAGUE. ZIJN FOCUS LIGT VOORNAMELIJK OP FYSIEKE ONTWIKKELING EN PRESTATIES. TEVENS IS HIJ DE ONTWIKKELAAR VAN HET ‘CONTROL-CHAOS CONTINUUM’.
DIT FRAMEWORK, WELKE VIJF FASES BESCHRIJFT HOE DE VELDREVALIDATIE NA EEN VOETBALBLESSURE OPGEBOUWD KAN WORDEN, STAAT CENTRAAL BINNEN DE WORKSHOP. DE THEORETISCHE ACHTERGROND,
DE TOEPASSING EN HET PRAKTISCHE ASPECT ZULLEN ALLEN AAN BOD KOMEN TIJDENS DE WORKSHOP.
reviews

Nick van der Horst
Meet the soccerdoc
Nick van der Horst behaalde zijn diploma fysiotherapie in 2007 aan de Hogeschool Utrecht. Hij werkte 10 jaar lang als sportfysiotherapeut/echografist/docent bij het Academie Instituut te Utrecht. Daarna heeft hij de overstap gemaakt naar waar zijn hart ligt, het professionele voetbal. Hij heeft twee jaar als sportfysiotherapeut en hoofd van de medische staf bij Go Ahead Eagles in Deventer gewerkt. Momenteel is is Nick werkzaam bij de KNVB. Zijn onderzoeks-activiteiten zijn gefocust op de voetbal-medische zorg. In 2017 behaalde hij zijn doctoraal na het verdedigen van zijn proefschrift ‘Prevention of hamstring injuries in male soccer’.
Part 2: Post-injury deficits and posture

Blogger: Raúl Gómez
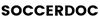
Eccentric training has been shown to be one of the most effective interventions in the rehabilitation and prevention of hamstring injuries. However, an injured muscle may not have the ability to adapt to an early eccentric stimulus and there is a risk of creating muscle imbalances that cause chronic pain or increase the risk of serious injuries such as the anterior cruciate ligament (Buckthorpe, et al., 2021). Therefore, before performing high intensity eccentric exercises with external loads, we must be sure that the football player’s movement is correct and efficient (Image 1). In this way, we will achieve optimal training adaptations and the football player will be able to return to competition with minimal risk of re-injury.
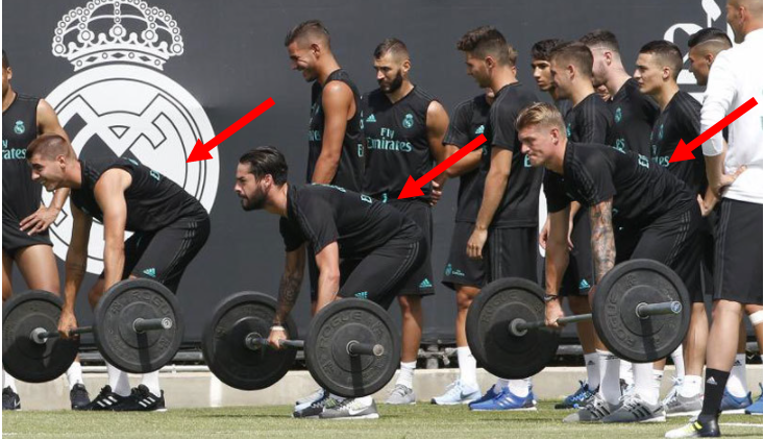
Image 1. Incorrect exercise technique. The lumbar muscles are not in a good position (lumbar flexion) to contract efficiently during hip extension, causing increased shear forces in the spine. In addition, posterior pelvic tilt shortens the hamstring muscles, limiting the eccentric stimulus during the execution of the exercise.
Knowing the anatomy and biomechanics of the hamstrings is a great help in treating their injuries: Part 1
Muscle healing process
After injury, the muscle goes through a complex recovery process and, although in each phase we will use different tests to ensure that everything is going in the right direction, we must know the basic concepts about muscle healing. It is important to know that not only muscle fibers are damaged, but also connective and neural tissue (Bayer, et al., 2018) and blood vessels (Jarvinen, et al., 2013). During the rehabilitation process we will face problems associated with the loss of muscle function due to the damage of different tissues.
After injury, a degeneration phase of the damaged tissue occurs (This cellular process is called apoptosis) together with the formation of a new membrane that seals the muscle rupture (Jarvinen, et al., 2013) (Image 2). This phase is also accompanied by inflammation, which contributes to phagocytosis (a process in which cells ingest others) of damaged fibers and promotes the process of muscle repair and regeneration (Dueweke, et al., 2017)
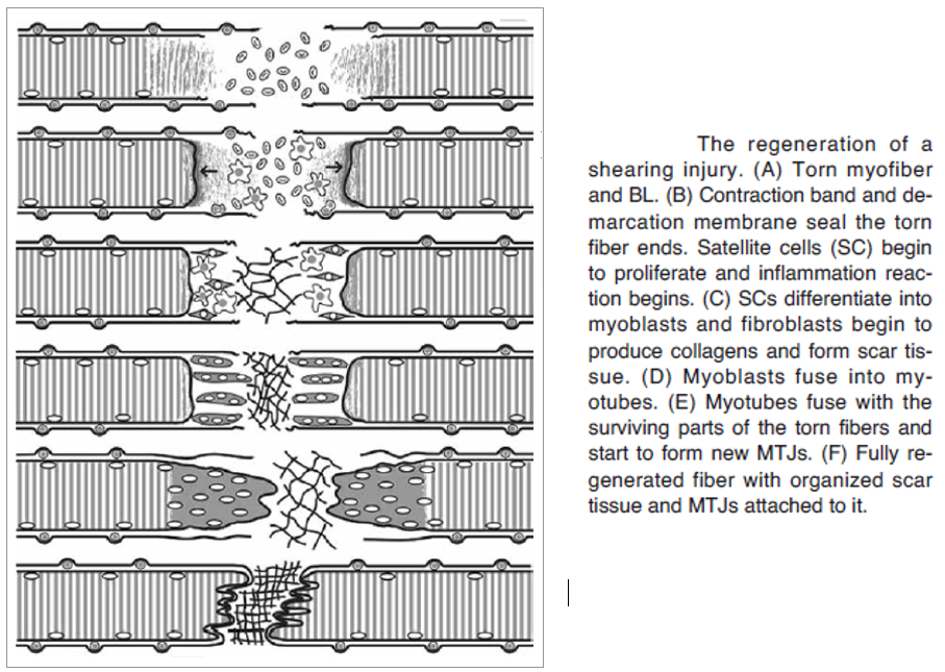
Image 2. Muscle repair process (Jarvinen, et al., 2013)
Within the first week after injury, the regeneration process begins. Growth factors are released (Gharaibeh, et al., 2012) and development of new muscle cells, regeneration of myofibrils and increase of capillaries for the revascularization of the previously damaged area occurs (Jarvinen, et al., 2013).
Finally, the remodelling phase occurs, the new tissue recovers its contractile function and fuse with the scar tissue formed after injury (Jarvinen, et al., 2013).
Recovery time can vary and depends on each person and characteristics of the injury. Svensson et al. (2016) carried out a review in which they compared image characteristics with the time required before return to play (RTP). Their results showed that the length of the tear in Magnetic Resonance Imaging (MRI) has a great correlation with the RTP time, the longer the length, the longer the time required for RTP. Injury to the biceps femoris (BF), presence of hematoma, proximity to the ischial tuberosity, and involvement of the proximal tendon are also factors that will increase the time required for RTP. Besides, stretch-type injuries (Askling & Saartok, 2008) and re-injuries (Valle, et al., 2017) will also need a longer rehabilitation time.
In the first phase, the main goal is the reduction of pain, inflammation and swelling (Dueweke, et al., 2017), while protecting the injured area (Hammond, et al., 2021). One of the most used methods is the RICE protocol (Rest, ice, compression and elevation), used with the aim of reducing bleeding in the injured area and, with this, reducing the hematoma, preventing further muscle retraction and reducing scar tissue (Jarvinen, et al., 2013). Some authors propose an alternative to the RICE rules by the POLICE rules (protection, optimal loading, ice, compression, and elevation), in which the early start of loading would be encouraged. Although it is still not entirely clear when rehabilitation should begin, authors as Bayer et al. (2018) has shown how an early start of rehabilitation (2 days) favors recovery and has a faster RTP than a delayed onset therapy (9 days). In addition, too long rest would impair and weaken the force transmission in the myotendinous junction, due to a reduction in its surface area because of the shortening of its folds (Rithamer & Rindom, 2021).
An early rehabilitation onset seems to be the best option for optimal muscle recovery, although we must be careful, since an excessive load and a prolongation of the inflammation time will impair recovery and increase the formation of scar tissue, which can cause problems such as muscle atrophy, loss of mobility and strength, and muscle inhibition (Bayer, et al., 2018).
There is not much research on compression and elevation treatments for hamstring tears, although the use of these types of therapies is very common. In the same way, despite the widespread use of heat and cold therapies, I was quite surprised that most of the recommendations are based on practical experience, since there is not a large amount of research regarding this type of therapy in humans (Dueweke, et al., 2017). Even so, I have been able to find several articles in which this type of therapy has been evaluated.
In a recent review, Kwiecien & McHugh (2021) showed contradictory results regarding the use of cold in musculoskeletal injuries. On the one hand, some authors support its use arguing that cryotherapy reduces the metabolic rate and inflammation and, consequently, reduces the proliferation and magnitude of secondary damage that occurs due to cell apoptosis in damaged fibers. But on the other hand, other researchers recommend avoiding the application of cold after injury or delayed onset muscle soreness (DOMS) since it could impair the natural healing process (which requires inflammation) and adaptations to training. Given these differences, the authors recommend using cryotherapy as soon as possible after injury, but avoiding its routine application for recovery after training, as this is likely to impair post-training muscle adaptations. The application of heat would be more advisable for the treatment of muscle soreness or joint pain and stiffness (Malanga, et al., 2015).
Cold application should be done in the first 24 hours, with the main goal of reducing intramuscular temperature for as long as possible to prevent the proliferation of secondary damage (Kwiecien & McHugh, 2021). Therefore, cold should be applied for a prolonged time during the first hours, as much as can be tolerated (Kwiecien & McHugh, 2021), but with caution so as not to cause problems such as skin burns or pain (Malanga, et al., 2015). After 24 hours, the application of cold will not have longer effect on reducing secondary damage, although it may have on reducing pain (Kwiecien & McHugh, 2021).
Post injury deficits
Although the goal of rehabilitation is to fully restore muscle function, the regenerative capacity of skeletal muscle is limited, so fibrotic tissue and scar formation will often occur (Gharaibeh, et al., 2012). This scar tissue is not elastic and can persist for months or become permanent (Fyfe, et al., 2013). This will alter muscle forces transmission and will increase strain of the tissues near the injury and the stiffness in the myotendinous junction, increasing re-injury risk (Silder, et al., 2010).
Image 3. Eccentric strength deficit during knee flexion (Buhmann, et al., 2020)
Due to the damage produced in the neural tissue, an activation of the protein degradation pathways will occur, causing muscle atrophy (Liu, et al., 2018). Moreover, denervation causes a decrease in capillaries, which leads to tissue devascularization (Bayer, et al., 2018). This lack of vascularization produces ischemic conditions in the muscle (lack of oxygen and nutritional materials in the cells due to the decrease in blood flow), which favors the formation of scar tissue and muscle dysfunction (Rithamer & Rindom, 2021) (Liu, et al., 2018).
All these changes in the muscle lead to loss of muscle function, causing deficits that, if not corrected, will cause chronic deficits and re-injuries, leaving the soccer player out of the game week after week.
Muscle strength is one of the functions that will be most affected. Several authors such as, for example, San Fillippo et al. (2013) indicate that after an injury, a protective muscular inhibition can occur that would limit the muscular forces to minimize the risk of suffering a second injury. This lack of muscle activation could be compensated by agonist muscles, creating an incorrect muscle activation pattern.
The greatest strength deficits after injury have been observed in the eccentric phase of knee flexion, together with the inability to achieve maximum muscle activation despite maximum effort (Buhmann, et al., 2020) (Image 3).
These results agree with those of many other investigations that find the same deficits, especially in positions where the knee is close to full extension, when the muscle is elongated (Sole, et al., 2011) (Maniar, et al., 2016). In this way, there is a change in the muscle strength-length relationship, with torque peaks generated in shorter muscle lengths (Fyfe, et al., 2013), which, in turn, will generate a greater deficit of strength in long length muscle positions, increasing the risk of injury.
Maniar et al. (2016), have also shown range of motion deficits after injury. Although in this article they conclude that deficits resolve in 20-50 days, in many cases these deficits become chronic. This lack of mobility, again, will create eccentric strength deficits.
The main idea is that after injury there are certain deficits that, if not resolved, can cause another injury, which consequently, will increase the deficits again, creating a vicious circle that in some cases can end up in chronic pain, muscle inhibition and atrophy. Thus, the body will create adaptations such as increased antagonistic activity or movement compensations, what will limit the injured muscle’s ability to gain eccentric strength and elongation in its fascicles (Buhmann et al., 2020) and can lead to serious injuries, either to the hamstrings or to different joints, such as the knee (Buckthorpe et al., 2021).
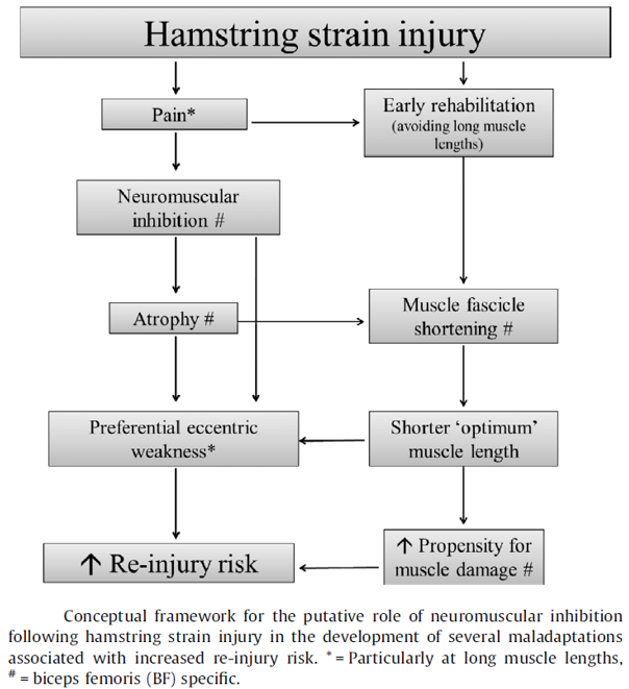
Maladaptations after hamstring injury (Fyfe, et al., 2013)
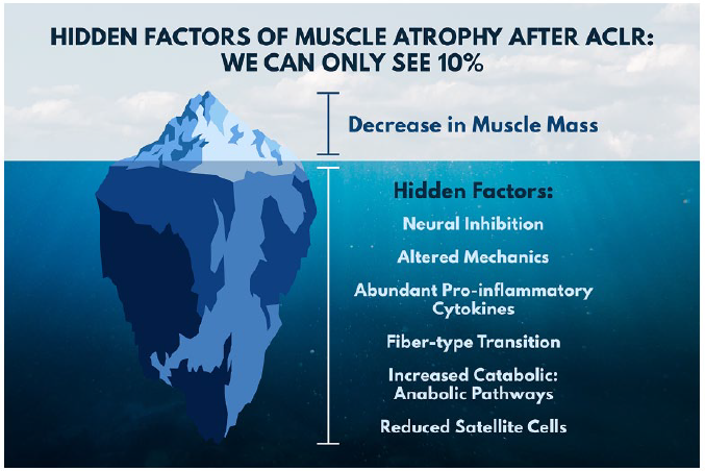
Image 5. Muscle atrophy factors (Lepley, et al.,2020)
Even though medical techniques are being developed to improve tissue after injury (Gharaibeh, et al., 2012) and therapies such as electromagnetic modalities already exist (Lepley, et al., 2020), physical therapy is one of the most effective tools in promoting muscle repair and regeneration. Exercise accelerates muscle healing by modulating the response of the immune system, releases growth factors, promotes vascularization, and reduces scar formation (Liu, et al., 2018). Therefore, a good planning of the rehabilitation will be key to obtain again maximum performance of the soccer player with a low risk of re-injury.
Posture
As I said in the previous post, the hamstrings are part of the posterior muscle chain (Wilke, et al., 2016) and a bad alignment of this chain will increase tension and injury risk, preventing correct adaptations to training (Due to incorrect techniques or compensations). Therefore, it is necessary to detect these deficits and work on them during strength training and soccer player’s rehabilitation.
Due to the highly repetitive nature of sport, our body will create movement patterns adapted to the actions we practice on a daily basis. This is particularly important in young people who play at top level, whose bodies are still developing, but are subjected to training loads that sometimes exceed the recovery capacity of their body. This, in the long term, can create postural disorders (especially of the spine) associated with pain and injuries (Stošić, et al., 2011).
For this reason, trainers and coaches, especially those who work with young athletes, should know how to evaluate and correct movement and posture. The development of an injury prevention plan for elite athletes should start at the youth academies, working on general motor skills and not just sport-specific skills.
Furthermore, strength training plans should be balanced between strengthening exercises and exercises aimed at improving arthro-muscular balance. For example, in most gyms, the use of pushing exercises such as push-ups or bench press is infinitely superior to pulling exercises such as rows or pull-ups, which in the long term will increase thoracic kyphosis. The same occurs with dominant knee and hip exercises, most are aimed at developing quadriceps power (Squat, leg extension, leg press …) with much less use of other exercises to strengthen the posterior chain (Deadlift, Hip Thrust, Back extension…). Considering that soccer itself already overstimulates the anterior thigh muscles, this training approach is the perfect method to create postural disorders.
Posture assessment, both static and dynamic, has aroused great interest in recent years due to the work of specialists such as Shirley Sahrmann, Gray Cook or Mike Boyle, although previously, Vladimir Janda was one of the key figures in movement-based injury rehabilitation. The main idea is that incorrect posture can affect force production quality and application and efficiency of movement, increasing the risk of suffering musculoskeletal injuries (Kritz & Cronin, 2008). In hamstring injuries, alterations in the sagittal plane are associated with the highest risk of injury.
Lower crossed syndrome
This movement syndrome, initially described by Dr. Janda and also known as pelvic crossed syndrome, is characterized by over-activation and stiffness of the thoracolumbar extensors and hip flexors, together with weakness of the abdominal and gluteal muscles (Das, et al., 2017). This movement pattern is related to increased anterior pelvic tilt, lumbar lordosis, lumbar lateral tilt, lateral leg rotation, and knee hyperextension.
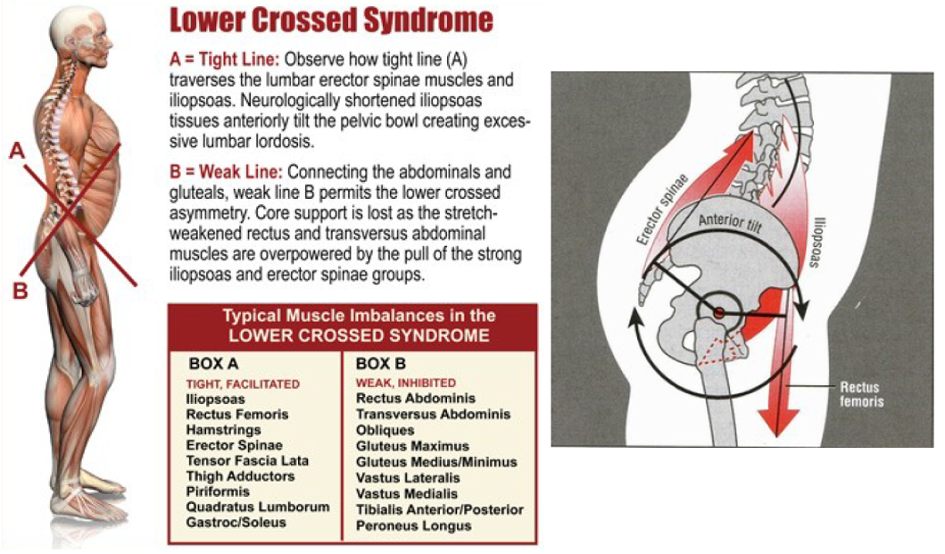
Image 6. Lower crossed syndrome and anterior pelvic tilt
Several of these factors, such as anterior pelvic tilt, leg rotation (Daly, et al., 2016), and increased lumbar lordosis (Mendiguchia, et al., 2020) have been related to hamstring injuries and low back pain.
In soccer, it is a very common pattern due to the demands of high intensity running. The increased anterior pelvic tilt increases hip extension range of motion, allowing the athlete to apply force for a longer time (Kritz & Cronin, 2008), thus compensating for the lack of force of the hip extensors, usually from the gluteus maximus. A training program focused on improving hip and trunk muscles strength and motor control, along with improving hip mobility and relaxation of the lumbar extensors has been shown to be effective in improving the incorrect movement patterns of this syndrome (Mendiguchia, et al., 2020).
Upper crossed syndrome
Pelvic and spinal biomechanics are closely related (Oxland, 2016) and movement disorders in one part will affect the rest of the structures. A poor alignment of hip and lower back will affect the position of the cervical and thoracic area and vice versa. One of the most common movement deficits nowadays is thoracic hyperkyphosis with forward head and rounded shoulders. Due to the excessive use of computers and mobile phones, we maintain injurious postures for hours every day. This can create a postural disorder known as upper crossed syndrome (Image 7), defined as hyperactivity and/or stiffness of the upper trapezius, pectoralis major, and levator scapulae, combined with weakness of rhomboid, serratus anterior, middle and lower trapezius, as well as the deep cervical flexors, in particular the scalene muscles (Ranđelović, et al., 2020).
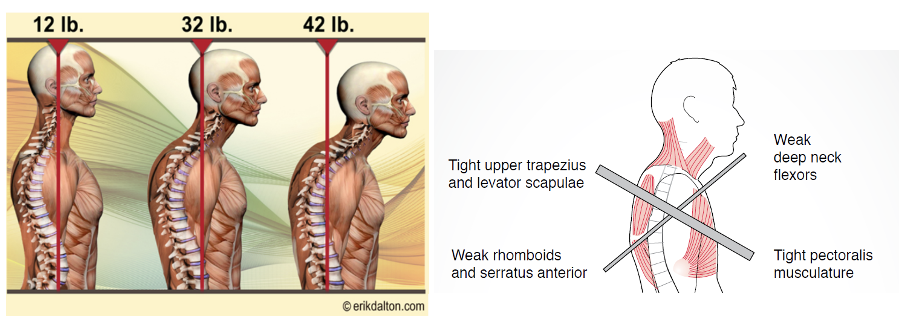
Image 7. Upper crossed syndrome (Left) (Muscolino, 2015). increased relative load due to head misalignment (Right)
This syndrome can cause neck, shoulder, or back injuries and scapular movement disorders (Ranđelović, et al., 2020). In people with forward head posture, imbalances in the activity of the neck, shoulder and back muscles have been observed during actions we perform daily. For example, Alowa & Elsayed (2021) showed a significant increase in the activity of the cervical musculature with the lifting of a weight of 5 kg in people with a forward head posture compared to people with correct alignment. In this same study, a trend towards greater activity of the thoracic and lumbar muscles was observed, although not significant.
Due to poor positioning of the head, shoulders and back, force transmission from the neck and thoracic spine will cause increased tension in the lumbar area (Rathore, et al., 2014). Consequently, the pelvis will also be affected, which might increase hamstring injury risk.
I think it is really important that we take these factors into account, not only after injury, but also in the development of preventive training and when planning a season with players of developing age. Young people grow up in an increasingly sedentary society with bad movement habits. For this reason, coaches must teach them to move well and develop a healthy lifestyle. Sometimes we are so busy dreaming of the great footballers that they are going to be in the future, that we forget to give them a solid foundation on which they can develop their abilities to the maximum.
The ability to generate power and be faster than your opponent can be key in a match, but the ability to decelerate and stabilize the body after maximum intensity action is key to both performance and injury prevention. If we want a football player to be able to use his full potential during competition, we must develop a perfect balance between his ability to generate force and his control over it.
References
Alowa, Z. & Elsayed, W., 2021. The impact of forward head posture on the electromyographic activity of the spinal muscles. Journal of Taibah University Medical Sciences, 16(2), pp. 224-230.
Areia, C. y otros, 2019. Neuromuscular changes in football players with previous hamstring injury. Clinical Biomechanics, Volumen 69, pp. 115-119.
Askling, C. & Saartok, T., 2008. Proximal hamstring strains of stretching type in different sports: Injury situations, clinical and magnetic resonance imaging characteristics and return to sport. The american journal of sports medicine, 10(10).
Bayer, M. y otros, 2018. Role of tissue perfusion, muscle strength recovery, and pain in rehabilitation after acute muscle strain injury. Scandinavian Journal of Medicine & Science in Sports, 28(12), p. 2579–2591.
Buckthorpe, M. y otros, 2021. Recommendations for hamstring function recovery after ACL reconstruction. Sports Medicine, Volumen 51, pp. 607-624.
Buhmann, R., Trajano, G., Kerr, G. & Shield, A., 2020. Voluntary activation and reflex responses after hamstring strain injury. Clinical Sciences, 52(9), p. 1862–1869.
Daly, C. y otros, 2016. The biomechanics of running in athletes with previous hamstring injury: A case-control study. Scadinavian Journal of medicine and science in sports, pp. 413-420.
Das, S. y otros, 2017. Prevalence of lower crossed syndrome in young adults: a cross sectional study. International Journal of Advanced Research, 5(6), pp. 2217-2228.
Dueweke, J., Awan, T. & Mendias, C., 2017. Regeneration of skeletal muscle following eccentric injury. Journal of Sport Rehabilitation, 26(2), pp. 171-179.
Fyfe, J., Opar, D., Williams, M. & Shield, A., 2013. The role of neuromuscular inhibition in hamstring strain injury recurrence. Journal of Electromyography and Kinesiology, Volumen 23, p. 523–530.
Gharaibeh, B. y otros, 2012. Biological Approaches to Improve Skeletal Muscle Healing after Injury and Disease. Birth Research Research, 96(1), p. 82–94.
Hammond, K., Kneer, L. & Cicinelli, P., 2021. Rehabilitation of soft tissue injuries of the hip and pelvis. Clinics in Sport Medicine, Volumen 40, p. 409–428.
Jarvinen, T., Jarvinen, M. & Kalimo, H., 2013. Regeneration of injured skeletal muscle after the injury. Muscles, Ligaments and Tendons Journal, 3(4), pp. 337-345.
Kritz, M. & Cronin, J., 2008. Static posture assessment screen of athletes: Benefits and considerations. Strength and Conditioning Journal, 30(5), pp. 18-27.
Kwiecien, S. & McHugh, M., 2021. The cold truth: the role of cryotherapy in the treatment of injury and recovery from exercise. European Journal of Applied Physiology.
Lepley, L., Davi, S., Burland, J. & Lepley, A., 2020. Muscle atrophy after ACL injury: Implications for clinical practice. Sports Health, 12(6), pp. 579-586.
Liu, J. y otros, 2018. Current methods for skeletal muscle tissue repair and regeneration. BioMed Research International, Volumen 2018.
Malanga, G., Yan, N. & Stark, J., 2015. Mechanisms and efficacy of heat and cold therapies for musculoskeletal injury. Postgraduate Medicine, pp. 1-9.
Maniar, N. y otros, 2016. Hamstring strength and flexibility after hamstring strain injury: a systematic review and meta-analysis. British Journal of Sport Medicine, 50(15), pp. 909-920.
Mcgill, S., 2009. Ultimate back fitness and performance. Fourth ed. Waterloo: Wabuno Publishers.
Mendiguchia, J. y otros, 2020. Training-induced changes in anterior pelvic tilt: Potential implications for hamstring strain injuries management. Journal of Sports Sciences.
Muscolino, J., 2015. Upper crossed syndrome. Journal of the Australian Traditional Medicine Society, 21(2), pp. 80-85.
Oxland, T., 2016. Fundamental biomechanics of the spine – What we have learned in the past 25 years and future directions. Journal of Biomechanics, Volumen 49, pp. 817-832.
Ranđelović, I., Jorgić, B., Antić, V. & Hadžović, M., 2020. Effects of exercise programs on upper crossed syndrome: A systematic review. Physical Education and Sport Through the Centuries, 7(2), pp. 152-168.
Rathore, y otros, 2014. A focused review – Thoracolumbar spine: Anatomy, biomechanics and clinical significance. Indian Journal of Clinical Anatomy and Physiology, 1(1), pp. 41-48.
Rithamer, J. & Rindom, M., 2021. The Myotendinous Junction—A vulnerable companion is sports. A narrative review. Frontiers in Physiology, Volumen 12.
San Fillippo, J. y otros, 2013. Hamstring strength and morphology progression after return to sport from injury. Medicine and Science in Sports and Exercise, 45(3), p. 448–454.
Silder, A., Reeder, S. & Thelen, D., 2010. The influence of prior hamstring injury on lengthening muscle tissue mechanics. Journal of Biomechanics, 43(12).
Sole, G., Milosavljevic, S., Nicholson, H. & Sullivan, J., 2011. Selective strength loss and decreased muscle activity in hamstring injury. Journal of Orthopaedic & Sports Physical Therapy, 41(5), pp. 354-363.
Stošić, D., Milenković, S. & Živković, D., 2011. The influence of sport on the development of postural disorders in athletes. Physical Education and Sport, 9(4), pp. 375-384.
Svensson, K. y otros, 2016. The correlation between the imaging characteristics of hamstring injury and time required before returning to sports: a literature review. Journal of Exercise Rehabilitation, 12(3), pp. 134-142.
Valle, X. y otros, 2017. Muscle injuries in sports: a new evidence-informedand expert consensus-based classification with clinical application. Sports Medicine, Volumen 47, p. 1241–1253.
Wilke, J., Krause, F., Vogt, L. & Banzer, W., 2016. What is evidence-based about myofascial chains: A systematic review. Archives of physical medicine and rehabilitation, pp. 454-461.