Student blog: ACL rehabilitation in elite football
VOETBAL MEDISCH SYMPOSIUM 2020
DE BEHANDELING VAN VOETBALBLESSURES
PRAKTISCHE WETENSCHAP
OP DE KNVB CAMPUS IN ZEIST VINDT KOMEND JAAR OPNIEUW HET VOETBALMEDISCH SYMPOSIUM PLAATS.
HET SYMPOSIUM IS DÉ PLEK OM COLLEGA’S BINNEN HET VOETBALMEDISCHE DOMEIN TE ONTMOETEN OF KENNIS OP TE DOEN VAN GERENOMMEERDE EXPERTS. EN DIE NIEUWSTE INNOVATIES TE ZIEN OP HET GEBIED VAN VOETBALMEDISCHE EN FYSIEKE PRESTATIES.
NA VORIG JAAR DE DIAGNOSTIEK VAN VOETBALBLESSURES BELICHT TE HEBBEN, ROLT DE BAL DIT JAAR VERDER NAAR DE BEHANDELING VAN VOETBALBLESSURES. HET INHOUDELIJKE PROGRAMMA BIEDT OPNIEUW SPREKERS DIE ZICH ONDERSCHEIDEN IN ZOWEL DE DAGELIJKSE ZORG VOOR DE VOETBALLERS ALS OP WETENSCHAPPELIJK GEBIED.
VOETBAL MEDISCHE WORKSHOP 2020
(VELD)REVALIDATIE NA EEN VOETBALBLESSURE
OP 4 MAART ZAL ER WEDEROM EEN WORKSHOP PLAATS VINDEN BIJ HET KNVB VOETBAL MEDISCH CENTRUM.
OOK DIT JAAR BELOOFD HET EEN OCHTENDVULLEND PROGRAMMA TE ZIJN WAAR VOORNAMELIJK (SPORT)FYSIOTHERAPEUTEN HUN KENNIS MEE KUNNEN UITBREIDEN.
TIJDENS DE WORKSHOP ZAL MATT TABERNER ZIJN KENNIS EN EXPERTICE MET DE DEELNEMERS GAAN DELEN. MATT TABERNER IS EEN ERVAREN CLINICUS DIE AL JAREN EINDVERANTWOORDELIJK IS VOOR DE REVALIDATIE VAN TOPVOETBALLERS IN DE PREMIER LEAGUE. ZIJN FOCUS LIGT VOORNAMELIJK OP FYSIEKE ONTWIKKELING EN PRESTATIES. TEVENS IS HIJ DE ONTWIKKELAAR VAN HET ‘CONTROL-CHAOS CONTINUUM’.
DIT FRAMEWORK, WELKE VIJF FASES BESCHRIJFT HOE DE VELDREVALIDATIE NA EEN VOETBALBLESSURE OPGEBOUWD KAN WORDEN, STAAT CENTRAAL BINNEN DE WORKSHOP. DE THEORETISCHE ACHTERGROND,
DE TOEPASSING EN HET PRAKTISCHE ASPECT ZULLEN ALLEN AAN BOD KOMEN TIJDENS DE WORKSHOP.
reviews

Nick van der Horst
Meet the soccerdoc
Nick van der Horst behaalde zijn diploma fysiotherapie in 2007 aan de Hogeschool Utrecht. Hij werkte 10 jaar lang als sportfysiotherapeut/echografist/docent bij het Academie Instituut te Utrecht. Daarna heeft hij de overstap gemaakt naar waar zijn hart ligt, het professionele voetbal. Hij heeft twee jaar als sportfysiotherapeut en hoofd van de medische staf bij Go Ahead Eagles in Deventer gewerkt. Momenteel is is Nick werkzaam bij de KNVB. Zijn onderzoeks-activiteiten zijn gefocust op de voetbal-medische zorg. In 2017 behaalde hij zijn doctoraal na het verdedigen van zijn proefschrift ‘Prevention of hamstring injuries in male soccer’.
Blogger: Cathal Corr
SoccerDoc stimulates knowledge development and personal development of anyone working within the field of Football Medicine. In addition to our bloggers who provide solid evidence-based coverage of certain topics,
we provide a platform for students to submit their work and share it with the SoccerDoc-community.
Feel free to share any knowledge, experiences and or comments below the blog to learn from each other.
Introduction
Anterior cruciate ligament injuries rank among the most prevalent and devastating injuries, affecting both amateur and elite athletes (van Melick, 2016). Despite the advancements in research and clinical practice, players playing at a professional level have a recurrence rate of 17.8% (Wright et al., 2007). Despite notable strides in research and clinical practices, professional players face a concerning recurrence rate of 17.8% (Wright et al., 2007).
Moreover, rerupture rates post-reconstruction range from 3-22% on the reconstructed ligament and 3-24% on the contralateral side, further complicating the rehabilitation process. The risk of a subsequent second ACL tear is not the only barrier to a successful return to sport, the return to preinjury level participation post ACL surgery is reported to be as low as 65%, underlining the multifaceted challenges athletes encounter in their journey back to peak performance (Ardern et al., 2015).
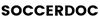
Against this backdrop, this blog endeavours to explore strategies for optimising ACL rehabilitation within the context of a multidisciplinary team (MDT) working within an elite football team setting. By delving into the workings of the MDT, we aim to elucidate how proactive organisational structures, effective rehabilitation planning, and open communication channels can bolster the success of rehabilitation efforts. Through these avenues, we seek to empower medical teams to navigate the complexities of ACL rehabilitation ultimately fostering the return-to-performance of the athletes with confidence and resilience.
Operational Structure
In elite football, a typical multidisciplinary team comprises five distinct departments, each playing a vital role in the management and preparation of players: coaches, medical team, performance team, data science team, and analysis team (Transfermarkt, 2023).
Each department brings specialised expertise and responsibilities to the table, collectively contributing to the optimisation of player performance and well-being.
Let’s briefly outline the roles and responsibilities associated with the two most prominent departments involved with the rehabilitation of a player with an ACL tear:
The Medical Department
The medical department consists of a sports medicine physician (club doctor) and typically 2-3 physiotherapists.
The Sports Medicine Physician
The sports medicine physician is typically the case manager and will oversee the rehabilitation period (Villa et al., 2019).
The Physiotherapist
The physiotherapists in the MDT will be responsible for the majority of the ACL rehabilitation. The regaining of range of motion, strength, power, hypertrophy, balance, and coordination are well-established and researched goals for the athlete to achieve under the guidance of the MDT; specifically the physiotherapist (Taberner et al., 2020).
The Performance Department
The performance department has a vital role to play in the reconditioning of the athlete back to the pre-injury level.
The strength and conditioning coach(s)
Here, the strength and conditioning coaches will reintroduce upper-body training and more dynamic and full-body movements once the initial protective phase has been completed (add more detail) at approximately 2-3 months post-surgery. The reconditioning of the body is crucial to regain the physical profile to compete at the highest level but also to build resilience to mitigate any further injuries (Bizzini et al., 2012).
The sports psychologist
However, the reconditioning of the mind is equally important and can be less straightforward (Ardern, 2015). Often overlooked, the psychological aspect of an ACL injury in an elite footballer cannot be underestimated. Mental training techniques to manage pain and reduce anxiety associated with injury are essential (Clement &Arvinen-Barrow, 2013). The sport psychologist provides screening and support for the player, with early identification of psychological barriers being crucial. Specific questionnaires to assess athletes’ fear, confidence, and perceptions of risk can help tailor interventions to their needs. This proactive approach can prevent psychological issues from hindering physical recovery (Ardern et al., 2013). Setting specific, measurable, achievable, relevant, and time-bound (SMART) goals helps athletes build confidence and stay motivated during their recovery (Ardern et al., 2022). The psychologist also encourages autonomy and control by advising the player to take an active role in their rehabilitation alongside the medical staff. Positive mental imagery, such as visualisation techniques, helps athletes imagine a successful return to the football pitch, reducing anxiety and fostering a positive mindset toward recovery and performance (Ardern et al., 2013). ACL rehabilitation is not a straightforward process, and setbacks are inevitable. The sport psychologist helps athletes develop coping strategies, emphasising relaxation exercises, cognitive-behavioural strategies, and ensuring adequate social support (Ardern et al., 2022).
Furthermore, it is my opinion that both the medical department and performance department may help with easing uncertainty, doubt, and fear of re-injury from the start. The medical and performance staff’s plan should give the players objective and measurable targets to hit. Players are natural competitors, and a long-term ACL injury rips away a big part of their life that motivates them daily. Measurable and objective short-term goals and targets can help feed that competitive urge and motivate the player. In addition to this, speaking with another player who has gone through the same long-term injury can allow the sharing of experiences, challenges, and solutions that we as non-playing staff members can not relate to.
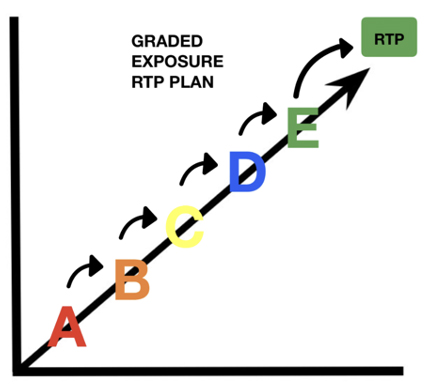
Image 2. Graded Exposure RTP Plan
Planning
A return to sport training plan should be completed within the first week of the ACL reconstruction. This plan should be coordinated and led by the ‘case manager’ (CM). The CM is typically the sports medicine physician within the organisation that leads the rehabilitation from start to finish. Their role is to give strategic and practical advice to the MDT on a daily basis and in key decision-making throughout the recovery process. When surgery is needed, the case manager liaises with the surgeon regarding the stages of tissue healing and the appropriate loading of the knee post-surgery (Villa et al., 2019). There are logistical factors such as travel requirements, budget, resources, MDT meeting schedule, and testing schedule. The recovery timeline should be forecast by taking into consideration the datasets of previous players who underwent ACL surgery. However, some covariates that need to be taken into consideration are previous knee injuries, the time of the season, and concurrent injuries such as a chondral injury, a meniscal tear or multi-ligament injuries (Jordan et al., 2015).
From my personal experience as a practitioner, a plan with clear milestones and progression/regression criteria enables the athlete to have a bird’s eye view of the rehabilitation plan and can help with any doubts or fears they may have. ACL rehabilitation is a long journey and there may be setbacks along the way.
Communication
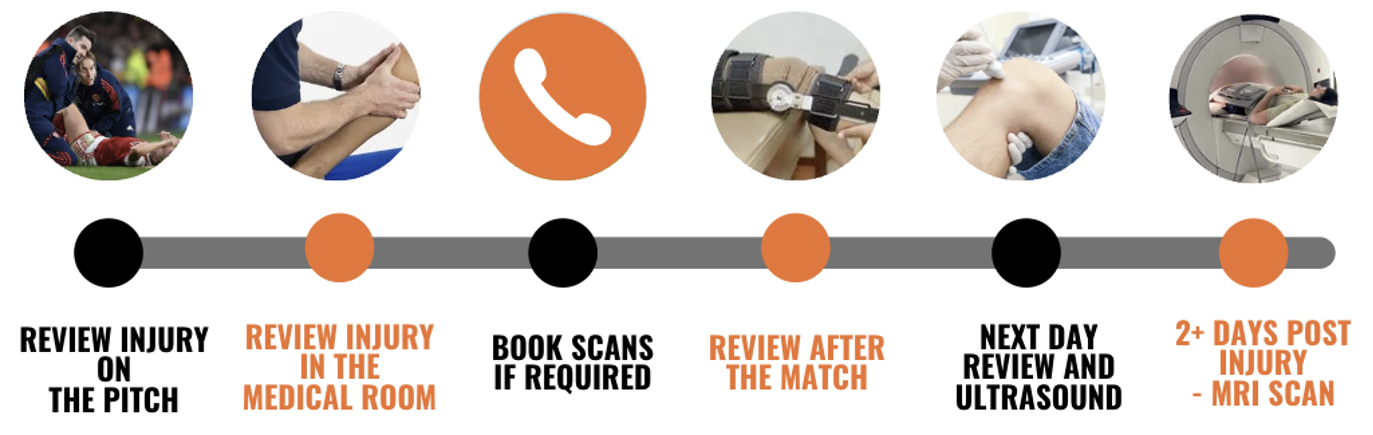
Acute stage
Acute injuries such as an ACL tear challenge the resilience and organisation of the MDT and emphasise the importance of teamwork and communication in such situations. On match days, at least one team doctor and at least one senior physiotherapist will make up the medical team on the sideline (The Football Association, 2023). In the event of an ACL tear, the medical team needs to be well-equipped to handle this scenario by coordinating their efforts effectively and following a clear and pre-planned protocol. Below I have illustrated the process of coordinating an ACL tear in training or on a match day.
Acute Injury protocol:
Image 3. Acute ACL Injury Protocol
Following the receipt of the imaging report, the CM follows a carefully controlled protocol. This allows discussion and communication of the injury, initially with one decision-maker, then with the Head Physio, a specialist if relevant, with the player, with the manager, director of football, medical team, logistics team and finally the board. Crucially, any media announcements should only be made after all the above individuals and teams have been informed and discussed the injury (Ahmad, n.d).
Use of Whatsapp
The day-to-day life of a footballer when not injured is carefully laid out and structured around team training, gym, tactical sessions and recovery. When our athlete is undergoing ACL rehabilitation, we should try to minimise the change of routine and help the athlete adjust to their new routine. The use of WhatsApp groups for rehabilitation can allow members of the medical team to quickly and effectively transfer information to athletes about training programmes, at-home rehabilitation and logistics around when and where to be day to day. Additionally, WhatsApp allows files, photos, and videos to be shared and stored for future reference. This can be of great benefit in the initial weeks post-surgery, as many players will travel abroad to undergo their surgery with their desired surgeon. WhatsApp messaging allows the player to relay information regarding their surgery, the status of their knee such as swelling, pain and range of motion and their overall well-being to the staff daily. It is important to note that this form of communication does not replace standard check-ins via video call or phone, but instead enhances the communication in between check-ins. Due to the understandable anxiety players feel around more sensitive information such as x-ray results and MRI scan results, this sharing of information should ideally be done in person or on the phone. This is not the purpose of the WhatsApp group. Continuous and effective communication is warranted within the caregivers’ team. Having a communication model (e.g., digital clinical records) and periodic (daily if necessary) meetings are the milestones of a well-organised service. Formal and informal communication is key to enhancing the relationship between the different players. The more you communicate within the team, the more you can maximise the patient or athlete’s perception of the recovery path and minimise the risk of misleading information to the patient (Ahmed et al., 2020). The use of WhatsApp groups does however bring the privacy of the patient and the ethical dilemma of sharing private medical information. Depending on the country, the laws around this topic vary, thus ensuring you are in line with your governing body and the specific privacy laws in your jurisdiction.
Conclusion
In conclusion, optimising ACL rehabilitation in professional football requires a comprehensive approach integrating structured multidisciplinary teamwork, meticulous planning, and open communication channels. By establishing clear operational structures within the multidisciplinary team, defining staff roles and responsibilities, and implementing effective planning strategies, such as coordinating return-to-sport training plans early on, the rehabilitation process can be streamlined for optimal outcomes. Moreover, leveraging communication tools like WhatsApp enhances the flow of information between medical staff and athletes, fostering a supportive environment crucial for successful recovery. With these strategies in place, the goal of leaving no stone unturned in ACL rehabilitation within elite football becomes more achievable, ensuring athletes can return to the field with confidence and resilience.
References
Football club doctor – An evolving role – injury rehab network event. Sterosport, https://sterosport.co.uk/dr-imtiaz-ahmad-football-club-doctor-an-evolving-role/
Ahmed, O. H., Carmody, S., Walker, L., & Ahmad, I. (2020). The need for speed! 10 ways that WhatsApp and instant messaging can enhance communication (and clinical care) in sports and exercise medicine. British Journal of Sports Medicine, 54(19), 1128-1129. https://doi.org/10.1136/bjsports-2019-101707
Ardern, C. L. (2015). Anterior cruciate ligament reconstruction—not exactly a one-way ticket back to the pre-injury level. Sports Health: A Multidisciplinary Approach, 7(3), 224-230. https://doi.org/10.1177/1941738115578131
Ardern, C. L., Hooper, N., O’Halloran, P., Webster, K. E., & Kvist, J. (2022). A psychological support intervention to help injured athletes “get back in the game”: design and development study. JMIR Formative Research, 6(8), e28851. https://doi.org/10.2196/28851
Ardern, C. L., Taylor, N. F., Feller, J. A., & Webster, K. E. (2013). A systematic review of the psychological factors associated with returning to sport following injury. British journal of sports medicine, 47(17), 1120–1126. https://doi.org/10.1136/bjsports-2012-091203
Arsenal FC – Staff. (n.d). Transfermarkt. Retrieved February 5, 2024, from https://www.transfermarkt.com/fc-arsenal/mitarbeit/verein/11
Bizzini, M., Hancock, D., & Impellizzeri, F. M. (2012). Suggestions from the field for return to sports participation following anterior cruciate ligament reconstruction: soccer. Journal of Orthopaedic & Sports Physical Therapy, 42(4), 304-312. https://doi.org/10.2519/jospt.2012.4005
Brinlee, A. W., Dickenson, S., Hunter‐Giordano, A., & Snyder‐Mackler, L. (2021). Acl reconstruction rehabilitation: clinical data, biologic healing, and criterion-based milestones to inform a return-to-sport guideline. Sports Health: A Multidisciplinary Approach, 14(5), 770-779. https://doi.org/10.1177/19417381211056873
Christakou, Α. and Lavallee, D. (2009). Rehabilitation from sports injuries: from theory to practice. Perspectives in Public Health, 129(3), 120-126. https://doi.org/10.1177/1466424008094802
Clement, D., & Arvinen-Barrow, M. (2013). Sport medicine team influences in psychological rehabilitation: A multidisciplinary approach. In M. Arvinen-Barrow & N. Walker (Eds.), The psychology of sport injury and rehabilitation(pp. 156–170). Routledge/Taylor & Francis Group.
Football Association. (2023). Premier League Medical regulations. Appointment of medical personnel, 2.1. theFA.com. https://www.thefa.com › rules-of-the-association
Jordan, M. J. and Aagaard, P. (2017). Anterior cruciate ligament injury/reinjury in alpine ski racing: a narrative review. Open Access Journal of Sports Medicine, Volume 8, 71-83. https://doi.org/10.2147/oajsm.s106699
Taberner, M., Dyk, N. v., Allen, T., Jain, N., Richter, C., Drust, B., … & Cohen, D. D. (2020). Physical preparation and return to performance of an elite female football player following ACL reconstruction: a journey to the FIFA women’s World Cup. BMJ Open Sport & Exercise Medicine, 6(1), e000843. https://doi.org/10.1136/bmjsem-2020-000843
Van Melick, N., Van Cingel, R., Brooijmans, F., Neeter, C., Van Tienen, T. G., Hullegie, W., & Sanden, M. W. N. D. (2016). Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. British Journal of Sports Medicine, 50(24),1506–1515. https://doi.org/10.1136/bjsports-2015-095898
Villa, F., Villa, S., & Mendes, J. E. (2019). Multidisciplinary sports medicine team. The Sports Medicine Physician, 3-11. https://doi.org/10.1007/978-3-030-10433-7_1
Wright, R. W., Dunn, W. R., Amendola, A., Andrish, J. T., Bergfeld, J. A., Kaeding, C. C., … & Spindler, K. P. (2007). Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction. The American Journal of Sports Medicine, 35(7), 1131-1134. https://doi.org/10.1177/0363546507301318